I don't mind sharing this. It's a clinical review my hospital did on one of my cases in 2010. For edification of the young ones! My physicist also didn't like that I (occasionally) wouldn't contour things. In the below case, I used a multi-field non-coplanar arrangement. In every single beam's eye view, I fixed the field size by adjusting the necessary jaw to completely cover the humerus and set the optimization to use fixed field sizes. Even though this "cut through the PTV" in some BEVs, the inverse optimization algorithm "handled it" and the dose to the PTV was homogenous and the max dose to the humerus was less than 10 Gy (this could only be confirmed by looking at each individual CT humerus slice though; read below). I didn't contour the brachial plexus because it more or less suffused the PTV region... and that was a primary reason I backed off on the Rx dose.
This same principle ("you don't have to contour it because you know it's spared") could not apply to brachial plexus in H&N, but most times in most of my H&N cases it is plainly obvious just from 1) mind's eye anatomic knowledge, and 2) understanding spatial distribution of the PTVs, that the uncontoured brachial plexus is not at risk from high dose RT. Ditto for lenses in whole brain plans etc etc etc. The primary reason to contour is to define where we want doses to go or not; the DVH is a fringe benefit of the contouring process but not the primary reason we contour. I never contour brachial plexus in HNSCC and have never had a brachial plexopathy as far as I know.
REVIEWER'S SUMMARY
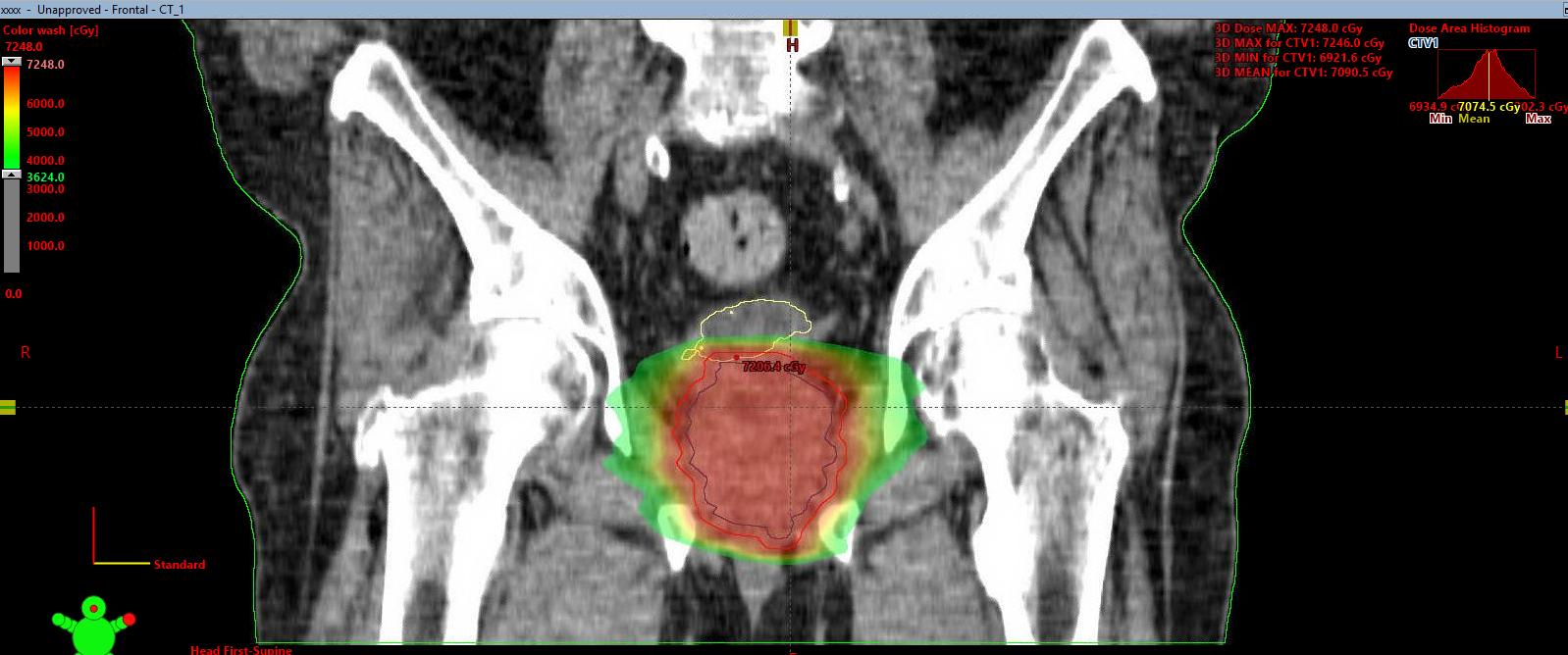
The patient was a 43-year-old man who presented with a recurrent mass involving his right axilla, upper arm and flank. By report, he had undergone previous resections of lipomas from this area in 2004, 2006 and 2007. A CT scan of the chest on February 2, 2010 revealed a 9.3cm x 8.9cm fatty mass in the right axilla, extending down the medial upper arm, with another component extending down the right lateral chest wall (reportedly roughly stable compared with a prior study on October 7, 2001). On May 3, 2010, the patient underwent a resection of a large T2aN0M0 liposarcoma involving the right axilla and flank at another facility. He was referred to the Practitioner for post-operative radiation treatment. The patient was seen in consultation by the Practitioner on May 26, 2010. The Practitioner states that “IMRT will be absolute [sic] necessary in this situation to spare the brachioplexus as maximally as possible versus 3D and lung as maximally as possible.”
The Practitioner’s initial treatment plan and orders dated May 27, 2010 documents that the Practitioner planned to deliver 66Gy in 33 fractions (fx) using IMRT to spare lung and soft tissue. The physician intent form, last modified on June 9, 2010, documents that the patient received 5840cGy in four (4) 200cGy fractions and 28 180cGy fractions. The radiation treatment summary dated July 30, 2010 states that the patient received a total dose of 58.4Gy, with a dose of 50Gy in 25 fractions (200cGy/fx) delivered to a wide area, including the operative bed, scar, and margin, with the preoperative tumor volume/operative bed receiving an additional 8-9 Gy. The dose was limited due to the proximity of the brachial plexus and humeral head to the clinical target volume. The patient was seen in follow-up on September 3, 2010.
The use of IMRT in this case was indicated given the initial extent to the patient’s disease and the post-operative surgical bed. Fusing the patient’s preoperative CT scan dated February 2, 2010 with the CT simulation was appropriate to accurately demarcate the planning treatment volume (PTV). The Practitioner’s goal to limit radiation dose to the lung, humerus, and brachial plexus was also appropriate given the location of the treatment area. The radiation dose actually delivered was slightly less than recommended, reportedly due to the need to limit radiation dose to normal tissues.
The cumulative dose volume histogram displays the radiation doses received by the clinical target volume (CTV), PTV, and right lung. During the Consultant’s review of the treatment plan on the Eclipse treatment planning system, it was noted that the right humerus was not separately contoured as an important organ (all bones including the humerus, scapula, ribs, and clavicle were outlined as one organ). Therefore, the radiation dose delivered to the humerus was not calculated or displayed on the dose volume histogram, and the humerus was not designated as a separate organ to limit radiation dose on the treatment plan. The failure to designate the humerus and humeral head as a separate organ may have resulted in an inferior treatment plan being chosen. The brachial plexus was also not separately contoured, but this would not be considered a deviation from the standard of care because of the potential difficulty in precisely localizing the brachial plexus. The Consultant also had potential concerns regarding the anterior-posterior and superior-inferior extent of the treatment volume, but a definitive opinion regarding the extent of the radiation fields would require a review of the pre-operative diagnostic films.
Overall, given the patient’s presenting extent of disease, the treatment delivered was reasonable and within the standard of care. However, the documentation of the plan, in particular the failure to calculate and limit the dose to the humerus, was suboptimal.
We got a chance to talk about the case. There was a transcript. Here's a portion of that:
REVIEWER: You said in your treatment summary that you limited dose to the humeral head and the brachial plexus. Do you remember that from your treatment summary?
ME: Yes.
REVIEWER: Well, you didn’t contour the humeral head or the brachial plexus in the planning system. Do you usually contour things in the planning system that you try to limit doses to?
ME: Well you can certainly identify them on the scan, right?
REVIEWER: Yep.
ME: So then you can identify your isodoses in the plan. And then if you find that your isodoses are acceptable in those regions, then you have limited doses to those structures.
REVIEWER: Right.
ME: So the simple explanation on that would be… and you might think this is a dumb example… but let’s say I’m doing whole brain irradiation. And I say, “I limited dose to the foot.” I might not contour the foot, but I have limited dose to the foot by just having radiation beams go to the head.
REVIEWER: But this isn’t that case. The brachial plexus and humeral head are very close by…
ME: But did you see the fluence maps?
REVIEWER: Yes.
ME: So you saw that I had intentionally fixed the field sizes in the plan to block the humeral head?
REVIEWER: Right.
ME: OK.
REVIEWER: Well at least in our planning system you don’t start a priori…
ME: But you certainly start a lot of things a priori… you choose beam angle, you choose beam energy…
REVIEWER: Right.
ME: … it wouldn’t have made a difference if I would have contoured these structures or not.
REVIEWER: Well you don’t know that. For example you might have contoured the structures and then told the computer to come up with a plan where it would have chosen different beam angles.
ME: Well… the computer never chooses beam angles. You know that right?
REVIEWER: Right.
ME: But you just said the computer would choose different beam angles.
REVIEWER: But you might have drawn some in that were weighted, or were next to things… I mean this is a unique case and very challenging.
ME: Right, very challenging. But I just want to get your sense of planning, because you do realize that when you are planning an IMRT case that you choose the beam angles, right, and not the computer?
REVIEWER: Yes. …
ME: Did you try a different plan?
REVIEWER: No, because I think it’s a quite challenging plan.
ME: Well did you think it was a good plan?
REVIEWER: I thought… it was a quite good plan…