I'm going through the above cited Red Journal paper on this,
DEFINE_ME and the separate paper published in PRO on the same topic,
DEFINE_ME.
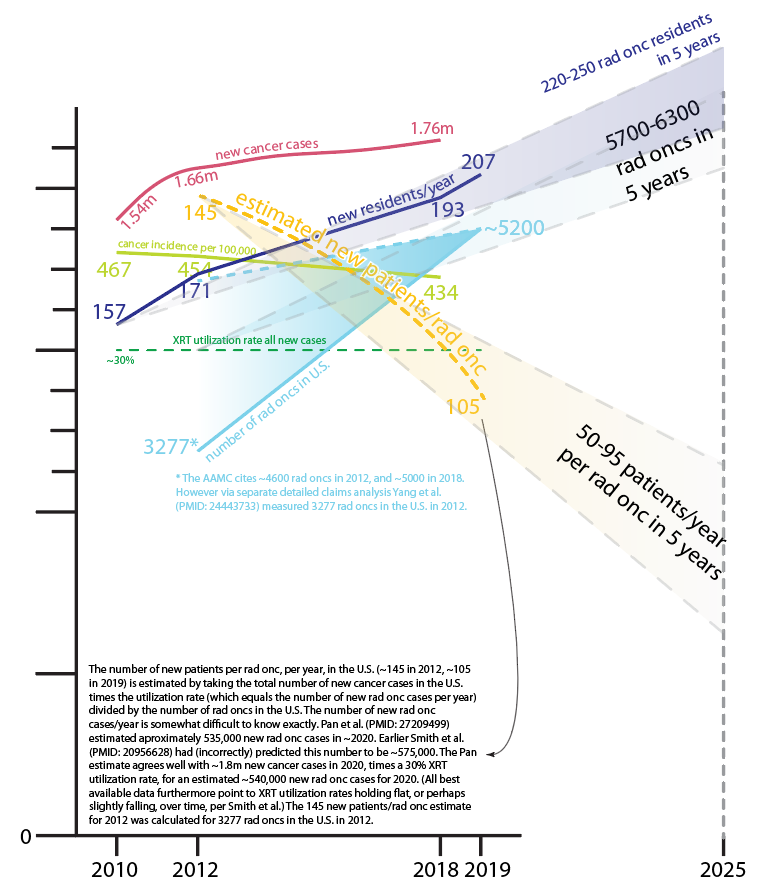
Both papers cite widely different statics regarding the number of practicing rad oncs.
From the Red Journal paper 4,948 MDs in 2013 and 5,415 MDs in 2017 (increase of 9.4%).
From the PRO paper paper 4,300 MDs in 2012 and 4,679 MDs in 2020 (increase of 9.0%).
Why are these figures so different and why is this such a hard thing to nail down?
From Red Journal paper's Methods section: "We utilized the Medicare Provider Enrollment, Chain, and Ownership System and Physician Compare databases to identify practices with radiation oncologists in 2013 and again in 2017. Individual practices were identified via unique individual or group practice tax identification numbers (TINs). Using this database, we were also able to obtain information on the location of each practice, as well as a listing of the National Provider Identifier (NPI) numbers of all radiation oncologists providing physician services within the practice. With these NPI numbers, we were able to link individual radiation oncologists at each practice to their billing records in the 2013 and 2017 Medicare Claims Carrier Files, which enumerates all physician service charges among a random subset of 20% of all Medicare beneficiaries. We further used NPI numbers to link to the Medicare Data on Provider Practice and Specialty database to obtain each radiation oncologist’s basic demographic information. We aggregated each practice’s zip code into specific Hospital Referral Regions (HRRs) as defined by the Dartmouth Atlas and extracted pertinent community characteristics as generated by the U.S. Census Bureau between the years 2011 and 2015.20 Table E1 provides further information on the specific datasets used and the linkages between each."
From the PRO paper's Methods section: "All data were obtained from the Physician Compare (PC) database. Given that this data set is publicly available and does not include patient-specific information, the study did not require institutional review board (IRB) approval. The PC database was created by the Centers for Medicare & Medicaid Services (CMS) in 2010 and is based on Medicare’s Provider Enrollment, Chain, and Ownership System (PECOS), a more comprehensive data set.22 The PC database contains information for health care providers who have either (1) newly registered in the PECOS system in the past 6 months, or (2) billed Medicare for at least 1 feefor-service reimbursement in the past 12 months; thus, all providers analyzed in our study meet these criteria. CMS uses billing claims to ensure that practice addresses are correct. The PC database is updated twice a month.23 In our study, we used data from the PC archive for 201224 (posted in September 2014) and April 2020.25 To identify RO physicians, the National Provider Identifier (NPI) was used. Those whose primary specialty was listed as RO were selected. The total number of individual practicing radiation oncologists and unique practices employing radiation oncologists were calculated for 2012 and 2020. A physician selection flowchart is provided in Fig. 1. Individual radiation oncologists were then categorized into bins based on their respective practice size (sizes 1-2, 3-9, 10-24, 25-49, 50-99, 100-499, and ≥500) using the same groupings as previous studies examining practice size consolidation.8,11 The number of individual radiation oncologists in each practice size category was determined for 2012 and 2020 using NPI (physician-level analysis). The number of unique practices in each practice size category for 2012 and 2020 was performed using a group’s Taxpayer Identification Number, or (TIN) (practice-level analysis). A Cochran-Armitage test for linear trend was used to determine whether the proportion of individual radiation oncologists or unique practices in each size category increased significantly between 2012 and 2020 for this test and tests in all subcategories. Nationwide data were divided into 4 US geographic census regions (Northeast, Midwest, South, and West), and the previously mentioned analysis was repeated for each. ....."

 ow.ly
ow.ly