- Joined
- Aug 20, 2021
- Messages
- 121
- Reaction score
- 52
- Points
- 201
- Fellow [Any Field]
Advertisement - Members don't see this ad
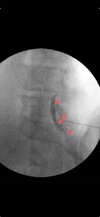
Hi all. I came across this picture during a review and the authors labeled this image as not epidural. I wanted to get folks thoughts on this. I admit I'm still a relatively new staff so If this looks this is blatantly not an epidural pattern I am happy to take pointers and learn. I feel fairly confident in identifying patterns that look classic like textbook images but sometimes for whatever reason (bad spines, volume of contrast used, could be technique too) I get patterns that don't look classic for epidural, subdural or otherwise. In fellowship for some reason they usually looked fairly obvious. I feel uncomfortable with these "in between" looking patterns and was wondering if people have shots of non-textbook looking epidural flows that are still epidural or tricky to identify patterns. All of the articles I find have pretty classic shots but none have in between. Even my colleagues who have 10 and 20+ years of experience disagree on some flows patterns when I ask them.