- Joined
- Dec 4, 2011
- Messages
- 1,905
- Reaction score
- 2,575
- Points
- 5,631
- Attending Physician
this makes sense physiologically but has it been shown to hold true in the literature? I was told and with limited reading have read that this doesn't pan out when you look at the evidence.TL;DR: CPAP and BiPAP are different and you need to know how to set the IPAP and EPAP in patients depending on their specific disease process.
I was also told something similar about "BiPAP vs CPAP increasing mortality in CHF" that didn't quite pan out in the literature. I think that it was a point raised in older studies that has been subsequently investigated and discredited.this makes sense physiologically but has it been shown to hold true in the literature? I was told and with limited reading have read that this doesn't pan out when you look at the evidence.
such as in
A comparison of continuous and bi-level positive airway pressure non-invasive ventilation in patients with acute cardiogenic pulmonary oedema: a meta-analysis
or
A comparison of bilevel and continuous positive airway pressure noninvasive ventilation in acute cardiogenic pulmonary edema. - PubMed - NCBI
I'll preface by saying that this is a huge pet peeve of mine.
Overall most EM physicians I've worked with do the same as you and just throw BiPAP on everyone regardless of the situation.
This is obviously the easiest option especially if you've got RTs around to manage these patients.
That being said I think this is bad practice for a couple of reasons:
1. CPAP and BiPAP are not the same thing and are meant for different patients.
I'll let Weingart explain below:
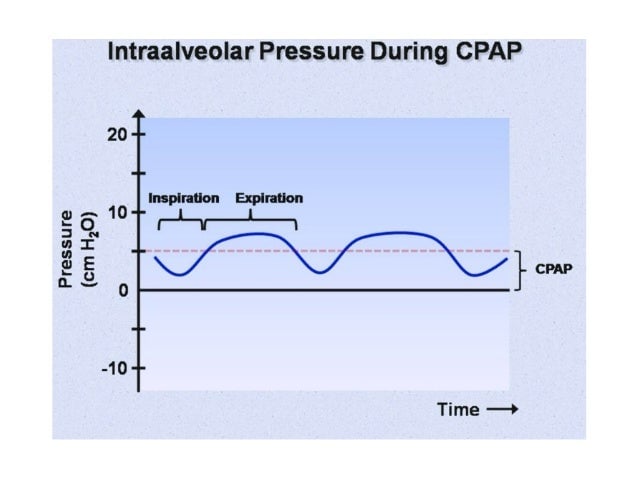
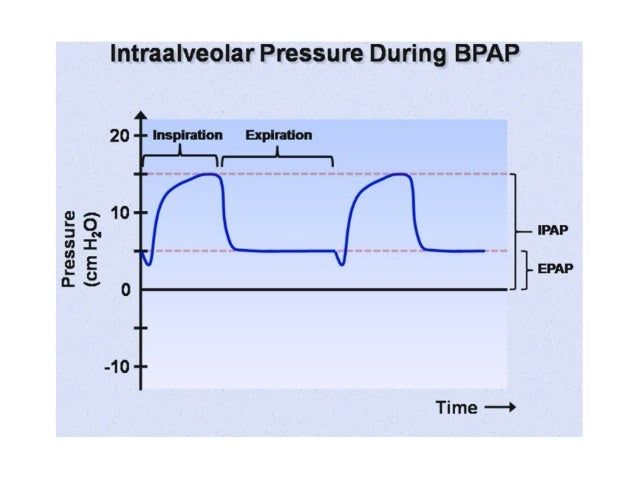
"If your patient has type I respiratory failure [inadequate oxygenation], then they need PEEP. They need CPAP (which is the same thing by a different name). CPAP (PEEP) fixes oxygenation failure. It recruits alveoli. It increases the matching between ventilation and perfusion. And if you have a pulmonary edema patient it decreases pre load and after load. Basically it does very good things for the patient with oxygenation failure. And you’ll see these good things almost immediately. And over the course of the next half hour or so they’ll keep getting better as alveoli pop open. So CPAP or PEEP is for oxygenation failure. Generally we start the setting at five and we can take it up to 15 if we need to. Now if you’re using a standalone machine then they’re going to call it EPAP which is the same thing as CPAP or PEEP. All those terms are synonymous. If the patient doesn’t have a ventilation issue, then they don’t need anything more than expiratory pressure. Just CPAP is all that they need. So don’t bother adding on inspiratory pressure. They don’t need it. If they have purely oxygenation problem then it is just CPAP. The patients with type II respiratory failure [inadequate ventilation], they are the patients who have problems with ventilation; like your asthma patients, and generally your COPD patients as well. What these patients really need is inspiratory pressure support. They don’t really need expiratory pressure. They already have auto peep Because they can’t get air out. So what these patients need is help getting air in. If you take these patients and put them on inspiratory pressure support, then they’ll start exchanging gas again. All of a sudden their oxygen saturation is back to hundred percent if you have them on supplemental FI02. And now the patient is getting their respiratory effort augmented by the machine. They still tell the machine when they need to breathe but the machine helps them get the air in. And they start looking good again. Same thing for your COPD patients. So these type II guys just need inspiratory pressure. And that is going to be IPAP when using a standalone machine and it’s going to be pressure support when using a ventilator. Generally I’ll also start that around five and work my way up to 15. Now most of these machines need just a little bit of Expiratory setting to keep the the masks open. So I’ll put that on 2 or 3 and not beyond that."
2. When you put everyone on BiPAP you're more likely to use the wrong settings.
If you place everyone on BiPAP there's a good chance you're also setting everyone to 10/5 or something along those lines. For the type I pulmonary edema patients this means that they're only getting 5 during expiration which is when they need the pressure the most because their alveoli are collapsing. At the same time for the type II asthma patients this means that they're also getting 5 during expiration which is when they need the pressure the least because they have trouble getting air out of their lungs. What I often notice is that people will just keep turning up both the IPAP and the EPAP when this happens which doesn't fix either probelm. As a result the patients often don't improve or only improve minimally after 30min on the machine and they end up getting intubated anyway.
TL;DR: CPAP and BiPAP are different and you need to know how to set the IPAP and EPAP in patients depending on their specific disease process.
I think you're wrong (and weingart) on two things above:
1) Patients with pure hypoxic respiratory failure do benefit from IPAP. Yes, it is the EPAP that helps address the hypoxemia, but (essentially) all patients with pure hypoxic respiratory failure (from an elevated A-a gradient, I.e. The ones you'd be using NIPPV for) will get tired and benefit from a touch of assistance.
I think you're wrong (and weingart) on two things above:
1) Patients with pure hypoxic respiratory failure do benefit from IPAP. Yes, it is the EPAP that helps address the hypoxemia, but (essentially) all patients with pure hypoxic respiratory failure (from an elevated A-a gradient, I.e. The ones you'd be using NIPPV for) will get tired and benefit from a touch of assistance.
2) Give the patients with severe auto-peep all the epap you want, it won't hurt them. Applying an artificial amount of Epap/cpap/peep that is below the intrinsic peep will have no effect on ventilation. In fact, if a patient who is autopeeping and having difficulty initiating the breath, the appropriate thing to do is actually raise the e-peep to approach the I-peep such that the patient becomes more synchronous. Sure, they don't need it on bipap, but you're not hurting them.
This.
Most of these pts requiring NIV in the ED (regardless of type 1&2 class failures) are tired and need ventilatory assistance or become tired and need ventilatory assistance. IPAP is useful for all these patients as well as the backup rate in case they suddenly lose their respiratory drive. The IPAP isn't going to hurt them and almost all of them are suffering from some element of respiratory fatigue. As long as you adjust EPAP accordingly based on the underlying pathology, you can essentially BiPAP everyone as long as you understand the settings and gradient. In essence, you can BiPAP both types of patients. Sure, sometimes I leave the pt on CPAP when they come in and EMS has initiated it or if there's an issue with pt-ventilation synchrony, etc.. but most of the time I'm using BiPAP.
Plus, last I checked there was no NVI literature showing the superiority of CPAP over BiPAP that was statistically significant.
This.
Most of these pts requiring NIV in the ED (regardless of type 1&2 class failures) are tired and need ventilatory assistance or become tired and need ventilatory assistance. IPAP is useful for all these patients as well as the backup rate in case they suddenly lose their respiratory drive. The IPAP isn't going to hurt them and almost all of them are suffering from some element of respiratory fatigue. As long as you adjust EPAP accordingly based on the underlying pathology, you can essentially BiPAP everyone as long as you understand the settings and gradient. In essence, you can BiPAP both types of patients. Sure, sometimes I leave the pt on CPAP when they come in and EMS has initiated it or if there's an issue with pt-ventilation synchrony, etc.. but most of the time I'm using BiPAP.
Plus, last I checked there was no NVI literature showing the superiority of CPAP over BiPAP that was statistically significant.
Technically speaking both CPAP and BiPAP provide IPAP and EPAP and thus both also provide ventilatory assistance and reduce work of breathing.
The main difference is that in CPAP the (EPAP>IPAP) while in BiPAP the (IPAP>EPAP). So in both cases you're getting increased inspiratory and expiratory pressures its just that in CPAP you're getting more EPAP while in BiPaP you're getting more IPAP. Patients with type I failure mainly need the higher EPAP to keep their alveoli open while patients with type 2 failure mainly need the IPAP to get air into their lungs. This is basically what Weingart was saying only in a more simplified manner.
LITFL has a great section on NIV including a video describing the above concepts on their website:
Non-Invasive Ventilation
Noninvasive Ventilation for the Critically Ill Patient
That's not correct. In CPAP, IPAP = EPAP. That's what makes it cpap.
I don't know any intensivist that I respect that uses cpap. It's a blunt instrument, whereas bipap allows you to fine tune what you're doing. Does it likely have any real influence on patient outcomes? Probably not, but it's much more physiologic, much more modifyable and much more elegant.
The literature is overall not very good but there is a Cochrane Review showing CPAP to be superior to BiPAP in acute cariogenic pulmonary edema.
Non-invasive positive pressure ventilation for cardiogenic pulmonary oedema | Cochrane
