- Joined
- Oct 23, 2019
- Messages
- 118
- Reaction score
- 29
- Points
- 120
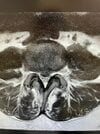
Young woman with L4-5 8-9mm posterior central protrusion with 8mm inferior subligamentous extrusion with severe central stenosis, thecal sac 5.7mm, with severe lateral recess narrowing. Pain is concordant with low back radiating to the hips, squeezing pain. Already doing medications to manage pain. Doesn’t want surgery yet....
Attached MRI images. Foramen doesn’t look too bad but severe L4-5 central stenosis. Inject bilateral L5-S1 TFESI….or go for the L4-5? I know there's going to be tons of opinions but wondering about your rationale.

Attached MRI images. Foramen doesn’t look too bad but severe L4-5 central stenosis. Inject bilateral L5-S1 TFESI….or go for the L4-5? I know there's going to be tons of opinions but wondering about your rationale.