- Joined
- Oct 23, 2019
- Messages
- 116
- Reaction score
- 27
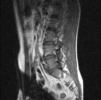
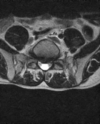
I have a young guy with low back pain radiating down the left leg in L5 dermatome with mild L5 EHL weakness (on going for several months).
Report & images attached:
L4-5: left paracentral & left foraminal herniated disc measures 15mm in vertical dimension with sequestration, severe spinal stenosis, narrowing of left neural foramen, facet hypertrophy.
L5-S1: 8mm central herniated disc causing severe spinal stenosis.
Previous pain doc tried to do a Left L4-5, L5-S1 TFESI but his contrast flow was suboptimal (don't think it made into epidural space).
He is already on medication but still having left sided radiating pain with L5 weakness.
Discussed surgery but he has a couple of summer trips coming up so holding off on surgery for now. I'd like to do another TFESI to give him some pain relief in the mean time.
What do you guys think?
1) repeat Left L4-5, L5-S1 TFESI (given poor contrast flow from prior pain doc's images)
2) Left L5-S1, S1 TFESI
Report & images attached:
L4-5: left paracentral & left foraminal herniated disc measures 15mm in vertical dimension with sequestration, severe spinal stenosis, narrowing of left neural foramen, facet hypertrophy.
L5-S1: 8mm central herniated disc causing severe spinal stenosis.
Previous pain doc tried to do a Left L4-5, L5-S1 TFESI but his contrast flow was suboptimal (don't think it made into epidural space).
He is already on medication but still having left sided radiating pain with L5 weakness.
Discussed surgery but he has a couple of summer trips coming up so holding off on surgery for now. I'd like to do another TFESI to give him some pain relief in the mean time.
What do you guys think?
1) repeat Left L4-5, L5-S1 TFESI (given poor contrast flow from prior pain doc's images)
2) Left L5-S1, S1 TFESI