There’s always going to be a difference between a gp interested in something vs. a specialist for sure. But it’s also true that a gp can be decent at certain things to do what they need to do for their patient as long as they are clear in their goals and know their limitations, and are transparent with their clients. And that can be the difference between life and death or treatment vs. no treatment for animals that are not going to ever go to referral. If follow-up to the $300 cytology and $700 ultrasound with a specialist is going to be followed with the fact that the client can’t afford any level of specialty care to treat whatever is found… it can make a huge difference for a gp to be able to search for specific things that they CAN do something about. I truly think that is exciting thing about gp. It’s not about let’s find everything you can about the patient’s situation often times. It’s about, can you find the one thing that you can do something about. And expanding your repertoire of the specific things you can confidently identify is huge. And being able to use that small piece of information as just one piece of the puzzle in interpreting your clinical situation is truly the art of a gp. What we do with that info is fundamentally different than the pathologist/radiologist, so the goal of the cytological and sonographic exam is also different. Sometimes it truly is that I need specialist interpretation before I can make a clinical decision, and it’s important for me to know and communicate that to the client.
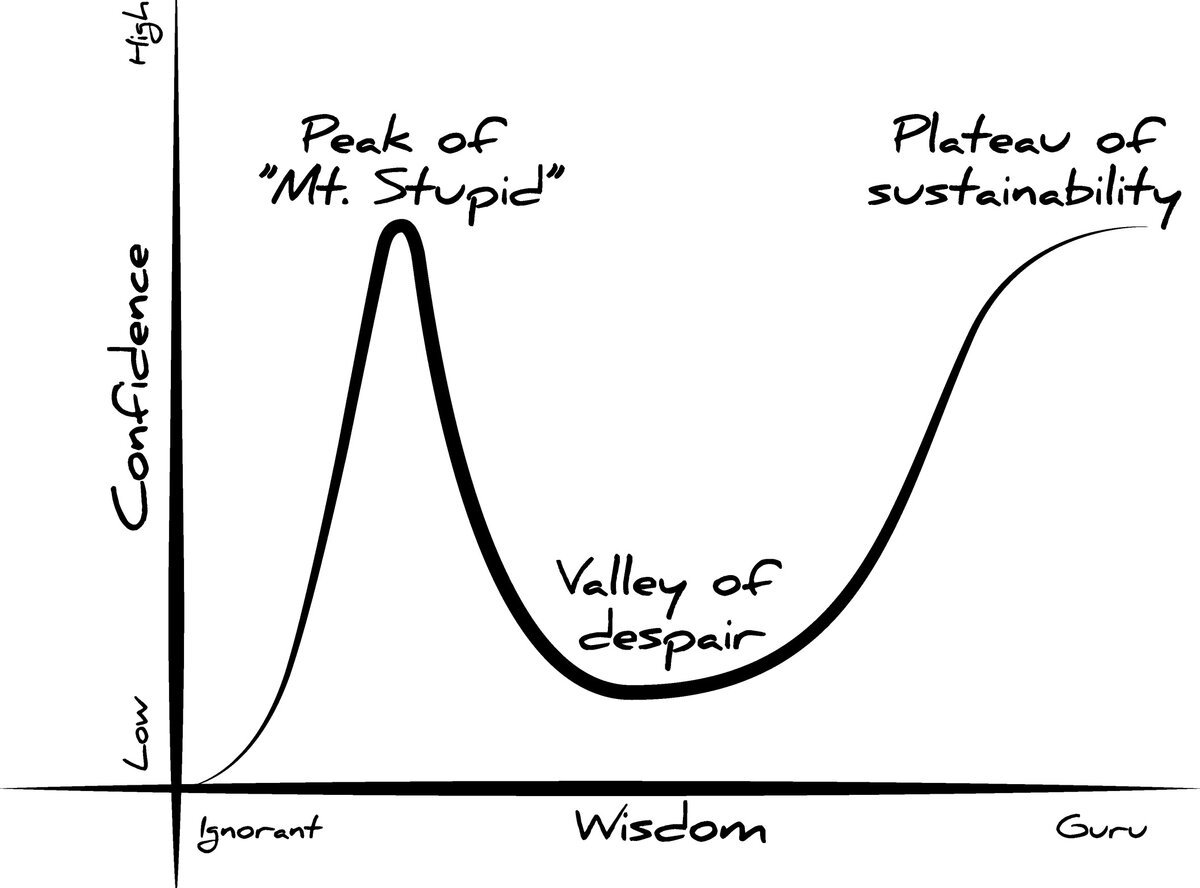
It is so important that a gp be past the peak of “mt. Stupid” when you offer these things, and appropriately use whatever knowledge/skills you have gained wisely and ensure your confidence level is appropriately good for whatever level of services you are competent at providing.
But like let’s talk about ultrasound and cytology since we’re at it. As a gp, I sure know my limits, and what I will put on paper in the record/tell the clients are a fraction of what I’m capable of seeing. I only state things that are super obvious, that I am SURE a radiologist/pathologist will agree with. I am never going to tell a client that the abdominal ultrasound is “unremarkable” or the lymph node is free of cancer. I absolutely hate when interns at the nearby ER feel so freaking ultrasound happy that they do not perform radiographs for intestinal obstructions or dyspneic/coughing animals, or uroliths, etc… before committing those patients to a plan. The patient gets referred back to me for definitive treatment or follow-up with nothing but a wild description of all the things they supposedly saw on ultrasound. Or they diagnose a pyo for a mildly distended uterus on ultrasound, when it doesn’t fit the clinical picture, and it’s an incidental hydrometra and surgery isn’t the appropriate next step for the sick patient.
But there is utility in being able to spot a large cell lymphoma on a smear, even if I can’t commit to small cell lymphoma vs reactive node if the client is not going to pursue an onco referral. And like was mentioned, there are some common diagnoses that gps can be good at identifying on cytology, as long as they can stick to those and also know when it is weird. There is utility in being able to confidently assess LA:Ao ratio and contractility - even if you don’t have the echo skills to diagnose the actual heart disease. I don’t need to be able to spot actual regurge to adequately assess, treat, and monitor that small dog with a progressive murmur acquired in middle age. Sure, that pet might live longer if their eventual CHF is managed by a cardiologist, but I can do a darn good job with appropriately combining plain film and t-fast and basic medical management. That pup does not need to be denied anesthesia earlier in the course of disease just because the client can’t afford both a dental procedure and a cardio consult. I can also assess for when that mmvd dog gets to stage B2 and start vetmedin to increase their lifespan. And that pup doesn’t have to be euthanized at time of going into CHF because they won’t go to the ER or see a cardiologist. Same with HCM. I might not be good enough to identify which cats need a beta blocker, but I can identify the ones that need blood thinners, and I can manage CHF.
Am I confident I will find a cryptorchid testicle in an animal on ultrasound? No. Me not finding it means nothing. But I’m really good at looking for inguinal ones no matter how tiny they are. That makes a huge difference for surgical planning. And I am not a boarded surgeon, but I am fairly good at exlaps for cryptorchids. If I can’t find it, it doesn’t mean it doesn’t exist, but I haven’t come across one yet I couldn’t find with a known hx of never having been neutered. I wouldn’t feel comfortable telling anyone the dog with unknown hx is neutered based on my explore. Knowing my limit matters.
With surgical procedures that are somewhat blurry in the maybe better with specialist territory, I will offer it especially if it’s life or death if it’s a skill I’m comfortable performing. But tell the owner they need to make up their decision and live with it. If something goes not well, we are talking euthanasia or even more expensive referral. If they will take the referral at that point, or if they are going to regret having me working my ass off to try my best to save their pet, then they need to go for referral now. If it truly is we are going to euthanize if I am not the person doing it, and they can afford and desire my level of care, and the client understands that I’m not a boarded surgeon/dentist, I will cut that PU or splenectomy or GDV or mandibular fx repair/partial mandibulectomy/rostral maxillectomy. I personally will not stretch for surgical procedures meant to increase qualify of life, but that a botched job on my part or a foreseeable complication can make things worse. So no thank you on things like TPLOs or a lot of ortho.
With that in mind, yes there actually is a lot that even a vet student can do to maximize their learning in school to start acquiring those skills. *START* being the key. But that head start can be invaluable if the student is invested. That student who goes out of their way to spend time with radiology and ER and gets mentored with actual probe driving time, they can learn a lot. Same with clin path cytology reading. Same with surgery. By the time I had graduated, I was down to under 30 min spays and I had cut Cherry eyes, R&A, cystotomy, pyo, and a few other things as the primary surgeon. You best believe I was a much more functional surgeon in gp right off the bat compared to many of my peers, and that set me up with enough confidence to pursue more procedures to build my skills in a mentored setting and with CE. Even if the student doesn’t know what they want to do with their lives yet, it’s never hurtful to gain hands on experience IMO. Don’t pigeon-hole yourself early on with any specialty, but a lot of the hands on skills can be helpful in many applications.
