Patients, such as diabetics, who have high blood-sugar levels before undergoing hip- or knee-replacement surgery are at increased risk of developing potentially life-threatening blood clots, according to a new study.
"The take-home message is that all patients should get their blood sugar under control before undergoing elective surgery," said the study's lead author, Dr. Boris Mraovic, an assistant professor of anesthesiology at Thomas Jefferson University in Philadelphia.
Mraovic's team examined records of 6,500 patients who underwent hip- or knee-replacement surgery at Thomas Jefferson University Hospital between 2003 and 2005. They identified 38 patients who had blood-glucose levels above 250 milligrams per deciliter during pre-operative testing and on the day of surgery. All but one of the patients were diabetic, which is defined as a fasting blood-glucose level above 126 mg/dl.
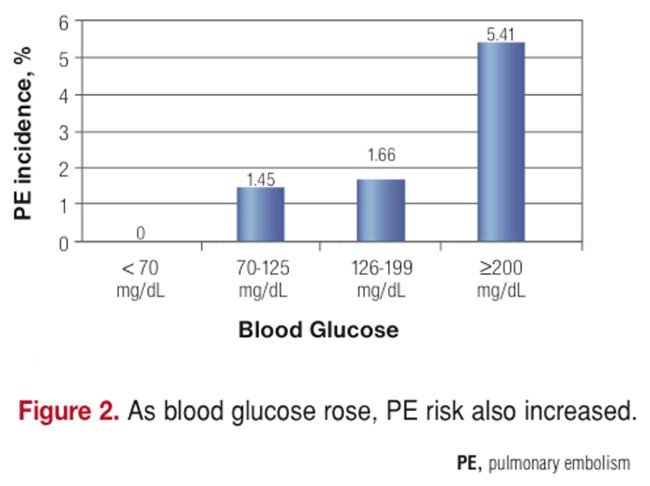
"We found that 10.5 percent of those with high blood sugar developed a pulmonary embolism compared to only 1.7 percent of the other patients," Mraovic said. "This rate is more than six times higher than we would expect to see in the general population."
Pulmonary embolism is a potentially life-threatening condition in which a blood clot forms in a vein and travels to the lungs. It's usually caused by clots that form in veins deep in the muscles of the legs or pelvic area, a condition known as deep-vein thrombosis.
Pulmonary embolism is more likely to develop after major orthopedic surgery than after other types of surgery. Nationwide, about 600,000 patients develop a pulmonary embolism each year and 200,000 of them die.
"Fortunately, none of the 38 patients in our study died," Mraovic said. "We treat pulmonary embolism aggressively."
Mraovic was expected to present his study findings Monday at the annual meeting of the American Society of Anesthesiologists, in Chicago.
"This is a fascinating study," said Dr. Samuel Goldhaber, a cardiologist at Brigham and Women's Hospital in Boston, who was not part of the study. "I'm not aware of previous studies linking poor glucose control with pulmonary embolism in patients undergoing surgery. So, this is the first one."
Although Goldhaber called the new research "intriguing and thought-provoking," he cautioned that it's premature to draw any major conclusions from it.
"This is just one exploratory study," he said. "It should prompt researchers to look through other databases to see if there's a similar relationship between high blood glucose levels and pulmonary embolism."
Previously, researchers didn't know if high blood sugar, per se, was an independent risk factor for pulmonary embolism in patients who undergo major orthopedic surgery. In fact, some research suggested otherwise. In 2002, a Mayo Clinic study of 19,293 such patients found that type 2 diabetes was not an independent risk factor for either deep-vein thrombosis or pulmonary embolism.
"The problem is, that study didn't examine high blood sugar," Mraovic said. "If you're diabetic, you can have normal blood sugar if you are taking medication."
Recent evidence shows that tight blood-sugar control leads to better results in patients who undergo cardiovascular surgery, Mraovic said. It's associated with improved survival, fewer infections, shorter hospital stays and lower costs.
Mraovic said guidelines are needed to limit elective surgery in patients who have high blood sugar. He favors guidelines that would require the postponement of such surgery until patients get their blood sugar under control. "At present, there are no such guidelines from surgical or anesthesia associations," he said.
Goldhaber disagreed. "I think more trials and studies are needed before we go that route," he said.
But he didn't dispute that well-controlled blood sugar should be the "rule of thumb" for all surgical patients, especially now that so many of them are diabetic. "Diabetes is becoming pandemic as part of the metabolic syndrome," Goldhaber said. "We need to focus a lot more attention on tightening blood-sugar control."
Mraovic said that additional studies are needed to confirm his results. He hopes to perform a prospective, randomized study of patients with high blood sugar to see if controlling their blood sugar before surgery lowers the risk of deep-vein thrombosis and pulmonary embolism.