- Joined
- Dec 12, 2003
- Messages
- 1,467
- Reaction score
- 948
Thought this might be a good teaching case for residents/fellows. My twist on this is instead of talking about intraop management, we can talk about preop assessment/plans prior to that (kind of like oral boards). This is a private practice case where you are solo (i.e. No resident, CRNA. Just you and your trusty Anesthesia Tech). You do all your own lines, TEE interpretation, etc. Here we go...
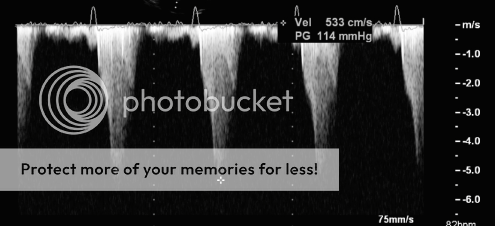
71 y/o male previous living at home with significant other experiencing angina with progression over past couple months. Comes in to see PCP 2 months ago, TTE was done which showed EF 50% with Mod-Severe AS. PCP schedules patient for nuclear stress test also which was done 1 week ago. Pt experienced intermittent and transient hypotension with this and "was extremely fatigued after this" while at home. Test showed anterolateral wall motion abnormalities. Pt presented later to ED that day with chief complaint of fatigue and angina. EKG does not show any ST/T wave changes, but does show a new Left BBB and BNP is in the 3000 range and tropnins are positive. Pt taken to Cath lab and found to have 99% LM and 100% occluded RCA (non-dominant). LV Ventriculography shows EF 10-15% now. Decision made to place Intra-aortic Balloon Pump (IABP). Angina improves with this. In addition, ICU places an arterial line, double lumen CVC, and Cordis. ICU staff unable to place PA Catheter as if was curling in RV. Pt has Carotid duplex that shows bl Mod-Severe Carotid Stenosis with poor vertebral flows. TTE shows EF 10-15% with low flow Aortic Stenosis classified as severe, with Moderate AI. TTE also shows mod-severe MR and TR, thought to be functional. Decision made to perform Right CEA prior to planned CABG/AVR/MVR/TVR. This was done successfully without issue and pt was extubated post-procedure. Pt had a headache post-op, but this has resolved. He is now POD #2 from this surgery and has been very well diuresed (20% of total body weight!). MR and TR are now Mild-Moderate. You go see him this morning and ICU nurse tells you he started getting stridor about two hours ago and his right neck is really swollen. He is talking and conversing with you. ICU has him on 2L O2 and NTG/Precedex gtt (Heparin gtt off for past two hours). Labs show low platelet count and low H/H. Creatinine, which had spiked on admission to 1.7 is now 1.0. TEG with platelet mapping shows only mild AA/ADP inhibition. IABP is set to 1:1 and his BP is 150/55 with HR in high 50s on NTG drip.
Now, I know some people on this board have been doing this stuff for a while and know the answers (i.e. Sevo, Hawaiian Bruin, etc), but try to give the residents/fellows a chance...
1) What is low-flow Aortic Stenosis? How do we diagnose this and why is it a bad idea to perform this test in this particular patient? How do we classify severity of Aortic Stenosis on Cardiac Cath versus Echo? How does his poor EF affect the Aortic Valve area calculation?
2) (Cardiac Fellows question) What is functional MR? How do you classify the different types of MR?
3) What are the contraindications to placing a PAC? What risks exist in this patient for placement? More importantly, are you going to place one?
4) How does an Intra-aortic Balloon Pump work? What is the proper position for the distal tip? When should it not be used? Why not place an Impella in this patient?
5) As above, the patient is now experiencing acute stridor that is clearly audible, but patient is talking normally per family and does not appear SOB. What do you want to do for him prior to surgery? Any prep for the OR?
Lets stop here for now. We can talk later about Intraop management and I will tell you what we did for this pt.
71 y/o male previous living at home with significant other experiencing angina with progression over past couple months. Comes in to see PCP 2 months ago, TTE was done which showed EF 50% with Mod-Severe AS. PCP schedules patient for nuclear stress test also which was done 1 week ago. Pt experienced intermittent and transient hypotension with this and "was extremely fatigued after this" while at home. Test showed anterolateral wall motion abnormalities. Pt presented later to ED that day with chief complaint of fatigue and angina. EKG does not show any ST/T wave changes, but does show a new Left BBB and BNP is in the 3000 range and tropnins are positive. Pt taken to Cath lab and found to have 99% LM and 100% occluded RCA (non-dominant). LV Ventriculography shows EF 10-15% now. Decision made to place Intra-aortic Balloon Pump (IABP). Angina improves with this. In addition, ICU places an arterial line, double lumen CVC, and Cordis. ICU staff unable to place PA Catheter as if was curling in RV. Pt has Carotid duplex that shows bl Mod-Severe Carotid Stenosis with poor vertebral flows. TTE shows EF 10-15% with low flow Aortic Stenosis classified as severe, with Moderate AI. TTE also shows mod-severe MR and TR, thought to be functional. Decision made to perform Right CEA prior to planned CABG/AVR/MVR/TVR. This was done successfully without issue and pt was extubated post-procedure. Pt had a headache post-op, but this has resolved. He is now POD #2 from this surgery and has been very well diuresed (20% of total body weight!). MR and TR are now Mild-Moderate. You go see him this morning and ICU nurse tells you he started getting stridor about two hours ago and his right neck is really swollen. He is talking and conversing with you. ICU has him on 2L O2 and NTG/Precedex gtt (Heparin gtt off for past two hours). Labs show low platelet count and low H/H. Creatinine, which had spiked on admission to 1.7 is now 1.0. TEG with platelet mapping shows only mild AA/ADP inhibition. IABP is set to 1:1 and his BP is 150/55 with HR in high 50s on NTG drip.
Now, I know some people on this board have been doing this stuff for a while and know the answers (i.e. Sevo, Hawaiian Bruin, etc), but try to give the residents/fellows a chance...
1) What is low-flow Aortic Stenosis? How do we diagnose this and why is it a bad idea to perform this test in this particular patient? How do we classify severity of Aortic Stenosis on Cardiac Cath versus Echo? How does his poor EF affect the Aortic Valve area calculation?
2) (Cardiac Fellows question) What is functional MR? How do you classify the different types of MR?
3) What are the contraindications to placing a PAC? What risks exist in this patient for placement? More importantly, are you going to place one?
4) How does an Intra-aortic Balloon Pump work? What is the proper position for the distal tip? When should it not be used? Why not place an Impella in this patient?
5) As above, the patient is now experiencing acute stridor that is clearly audible, but patient is talking normally per family and does not appear SOB. What do you want to do for him prior to surgery? Any prep for the OR?
Lets stop here for now. We can talk later about Intraop management and I will tell you what we did for this pt.