- Joined
- Apr 15, 2011
- Messages
- 907
- Reaction score
- 381
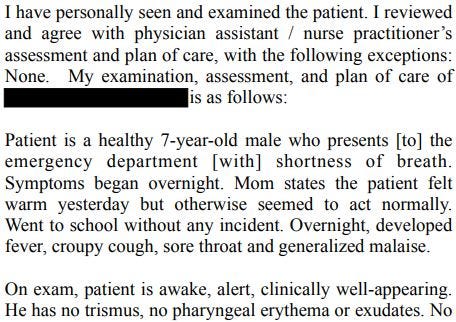
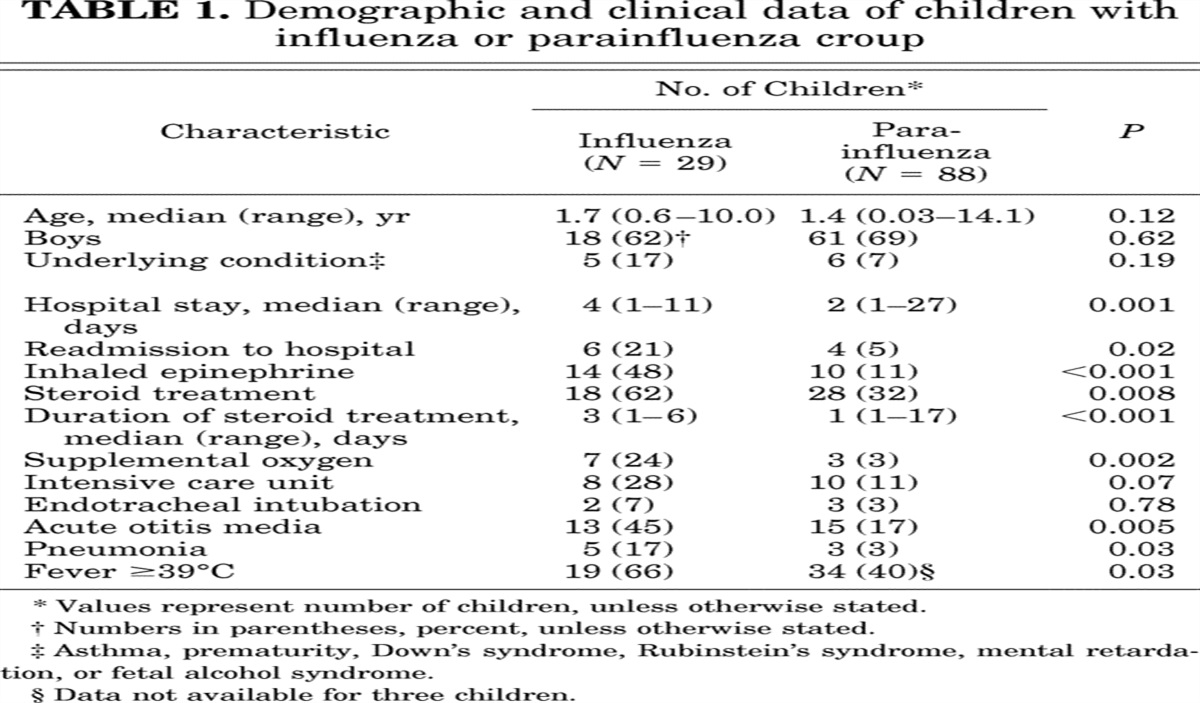
Tragic case. 7 yo with barky cough, benign presentation in the ED, diagnosed and treated for clinical croup, positve for flu B, later had a GAS necrotizing lung infection and fatality. Reading through the case, can happen to anyone, but was boiled my blood was reading through the plaintaiff's expert opinion.
IM physician, EM boarded, ACEP and SAEM member, apparently teaches at an EM residency program
- reports croup and influenza B cannot occur at the same time
- insists "marked deviation of care" for giving decadron which resulted in overwhelming GAS infiection
- should not have given dexamethasone for clinical croup until the results of the viral PCR, which "demonstrated a reckless indifference to pending test results and instituting proper treatment, which is both shocking and outrageous and well outside the boundaries of accepted standard care"
- saying that the documentaiton in note "We will give decadron" with the note signed after the completion of the visit, is "clearing inappropriate and and lacking in honesty" and "is extremely unusual and calls into question the chain of events"
- did not offer the patient the opporutnity to be evaluated by a pediatric specialist, did not inform the parent her child had been inappropriately treated with Decadron, nor speak with a pediatric specialist under that circumstance, as should have been done, "shocking departures from the recognition of patient right"
Would I have considered a CXR for a croupy presentation in a 7 year old who is slightly out of the normal croup range and who is flu positive? Maybe. I would have thought more about it, and it is unclear if a CXR would have even changed anything. But, there is nothing about the case remotely out of the standard of care in how it was treated. But this is one of the worse expert witness opinions I've seen (after that one surgery opinion that cited medscape). Expert witesses like this should be sanctioned by every society, and case referred to their department chairs.