- Joined
- Jul 27, 2010
- Messages
- 1,814
- Reaction score
- 1,526
Thought this may be an interesting study for the PTSD and DBT folk on the forum
 jamanetwork.com
jamanetwork.com
Dialectical Behavior Therapy for PTSD vs Cognitive Processing Therapy in Women Survivors of Childhood Abuse
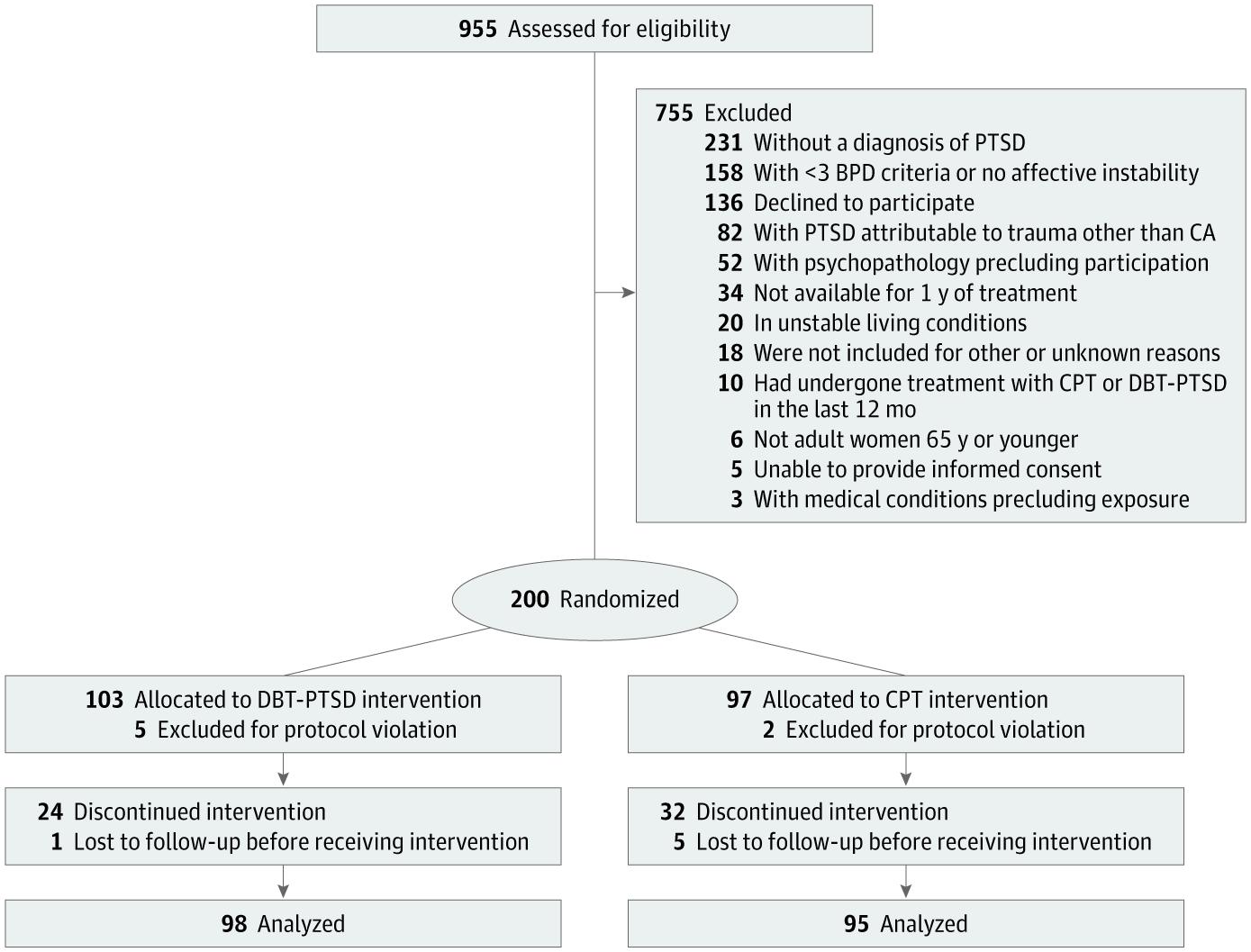
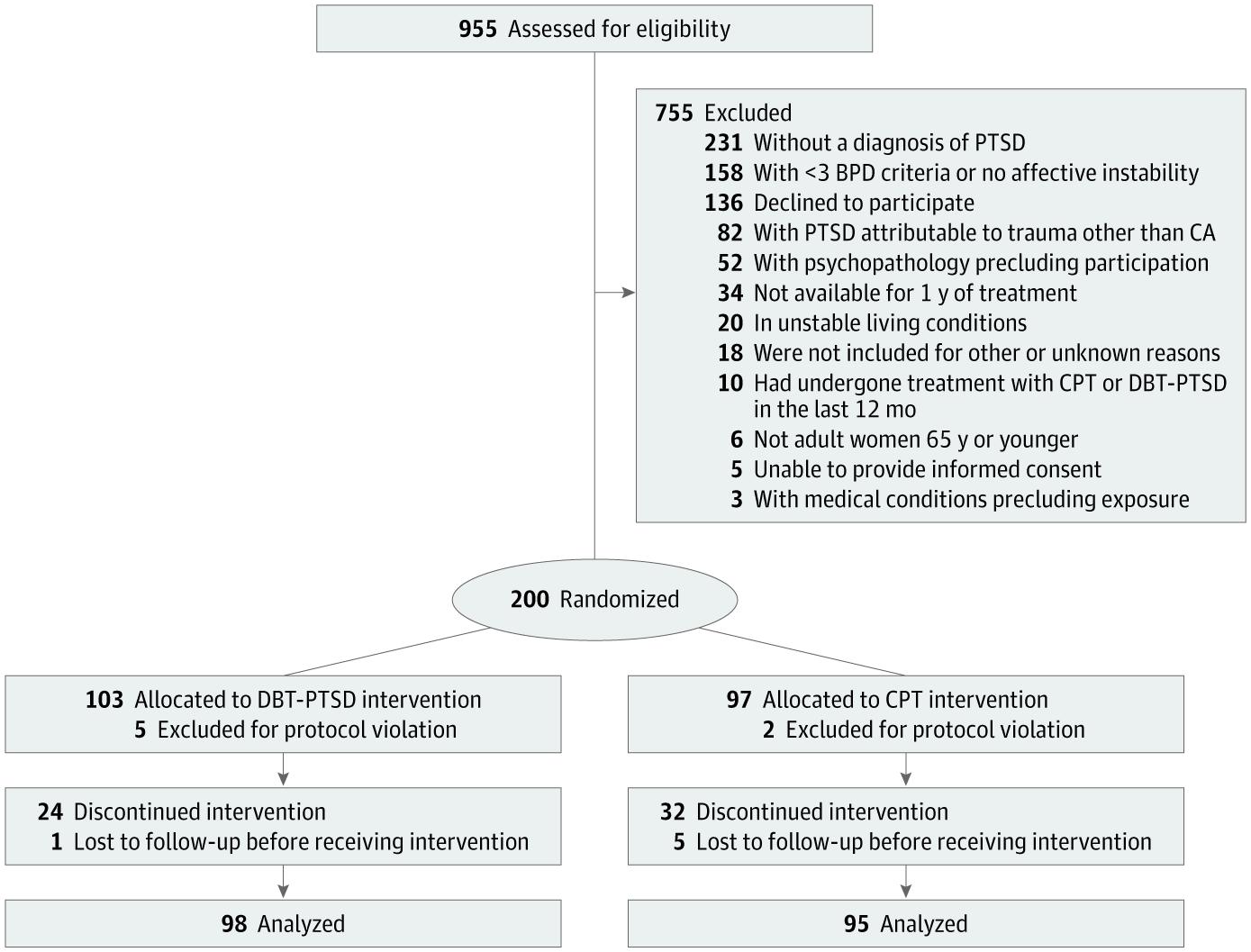
This randomized clinical trial compares the efficacy of 2 therapies for childhood abuse–associated posttraumatic stress disorder in women by randomizing participants to receive dialectical behavior therapy for posttraumatic stress disorder or cognitive processing therapy.
