- Joined
- Jul 12, 2004
- Messages
- 5,278
- Reaction score
- 4,969
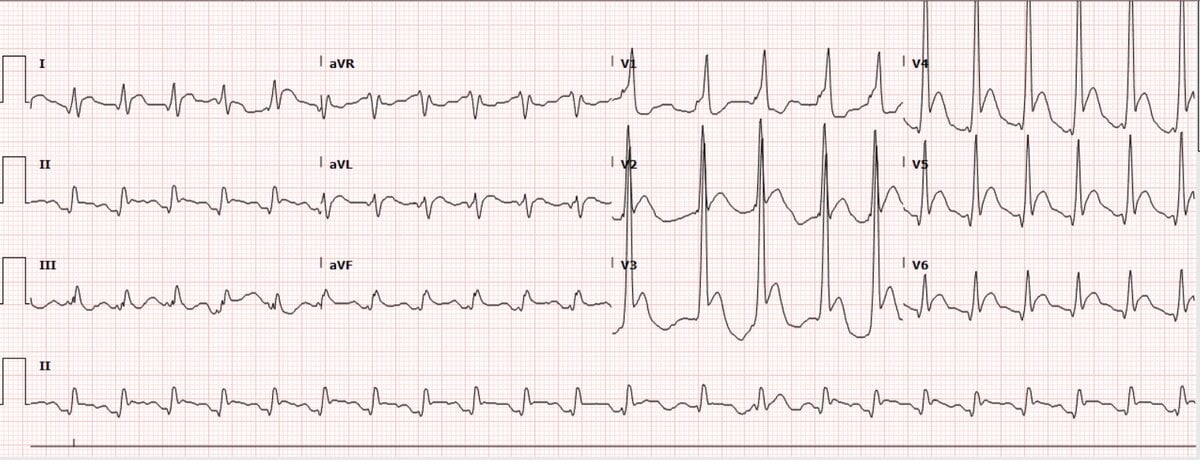
71 yo man with unknown PMH BIBA undergoing CPR. He has a witnessed syncopal event in a parking lot. First rhythm was VFib and was defibrillated by first responders. He underwent about 30 mins of CPR, received numerous ACLS meds, and I was able to get a pulse. The EKG below was done about 2 minutes post-ROSC.
Do you think this is a STEMI? Would you activate? (note these are two different questions as it's possible to answer "no" and "yes")
I will later discuss what happened.
Do you think this is a STEMI? Would you activate? (note these are two different questions as it's possible to answer "no" and "yes")
I will later discuss what happened.

