- Joined
- Jan 27, 2010
- Messages
- 431
- Reaction score
- 408
That’s for sharing.
What’s the rationale for not being overly aggressive about offering it? I imagine it’s because it’s not as slam dunk as other things we do.
Clinical judgement. I get a fair number of referrals for people who are still in the fringes of post-op pain or have been non-compliant with PT, etc. so I just don't start doing it for people because they are likely poor candidates. If they finish PT, compliant with conservative therapy, and continue to have pain then we will change plan to GNB RF. If the referral is for painful hardware or CRPS then wait at least 3 months post-op, failed Lyrica, etc.
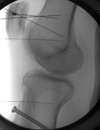
Do one GNB then RF. Bill 64624.