- Joined
- Jan 9, 2002
- Messages
- 6,517
- Reaction score
- 3,074
I've done thousands of cervical medial branch blocks and radiofrequency ablations. My needles go to the right place, and the final images look great. Excellent outcomes. No serious complications.
HOWEVER, I'm tired of agonizing over the patient positioning, excessive radiation exposure, and time.
I do my cervical medial branch blocks in the side lying position. That takes a good bit of time to set up properly. Should I convert to patient supine (from lateral approach) or prone (from posterior to anterior approach) to speed things up?
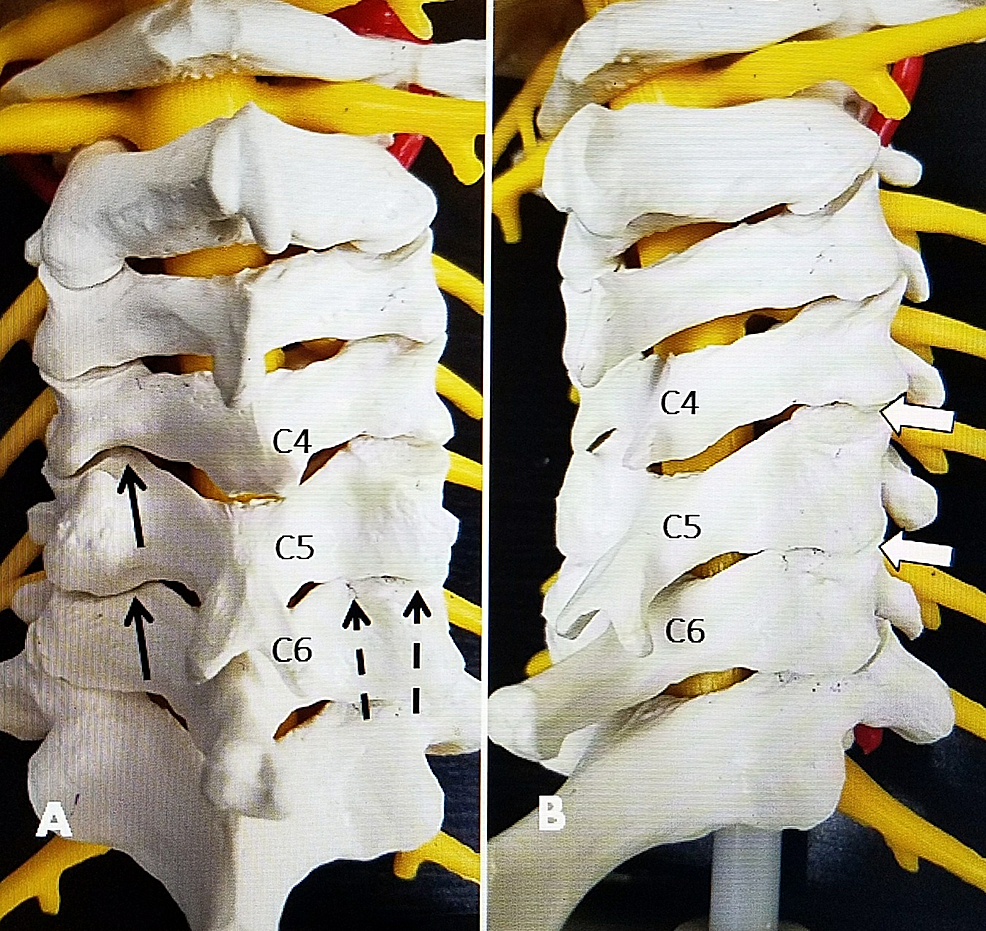
TON and C4 mb radiofrequency ablation frequently takes me a decent amount of time to image with patient prone and looking straight ahead. C5-7 go quickly in this position.
I've done patient prone with head rotated to contralateral side, which works nice for C4-7 but the rotation makes lateral views at TON and C4 difficult. For TON and C4, I've been toying with the idea of starting with head rotated to contralateral, placing needles down to pedicle, then manually rotating the patients head back to looking straight ahead to obtain a lateral view and advance further.
Any tips to make things more efficient appreciated.
I'm also open to ultrasound guided cervical medial branch blocks, if indeed insurance is reimbursing for them.
HOWEVER, I'm tired of agonizing over the patient positioning, excessive radiation exposure, and time.
I do my cervical medial branch blocks in the side lying position. That takes a good bit of time to set up properly. Should I convert to patient supine (from lateral approach) or prone (from posterior to anterior approach) to speed things up?
TON and C4 mb radiofrequency ablation frequently takes me a decent amount of time to image with patient prone and looking straight ahead. C5-7 go quickly in this position.
I've done patient prone with head rotated to contralateral side, which works nice for C4-7 but the rotation makes lateral views at TON and C4 difficult. For TON and C4, I've been toying with the idea of starting with head rotated to contralateral, placing needles down to pedicle, then manually rotating the patients head back to looking straight ahead to obtain a lateral view and advance further.
Any tips to make things more efficient appreciated.
I'm also open to ultrasound guided cervical medial branch blocks, if indeed insurance is reimbursing for them.
Last edited: