Like these ones?
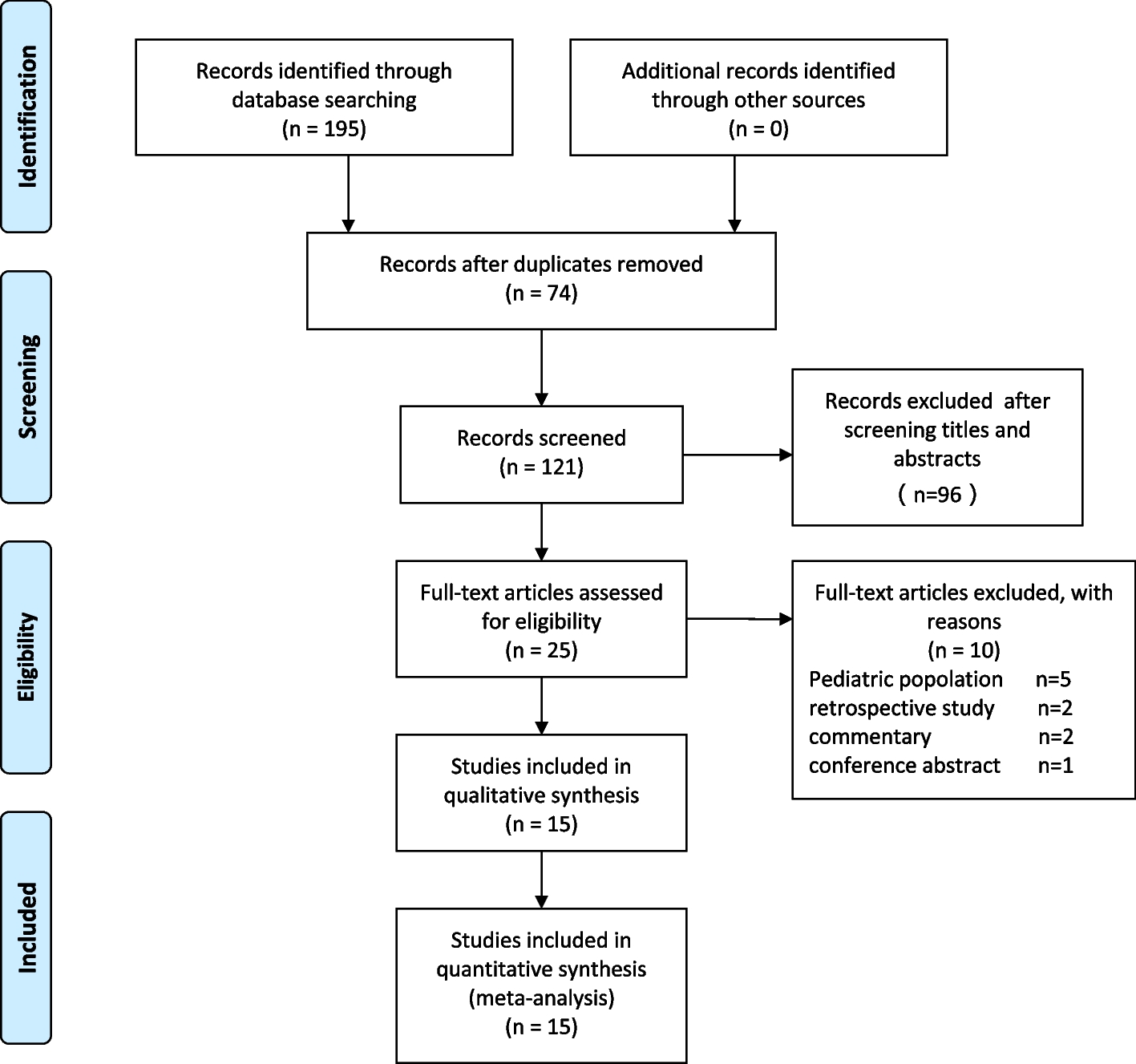
Ultrasound-guided Erector Spinae Plane Block (ESPB) has been increasingly applied in patients for postoperative analgesia. Its effectiveness remain uncertain. This meta-analysis aimed to determine the clinical efficacy of ultrasound-guided ESPB in adults ...

www.ncbi.nlm.nih.gov
Background Laparoscopic cholecystectomy is the gold standard surgical procedure for treating gallstone disease. Despite it being minimally invasive, various medications and methods are used to alleviate postoperative pain, and some patients still experience moderate-to-severe pain. This is a...
bmcanesthesiol.biomedcentral.com
Now have I meticulously reviewed every article? Nope. But generally speaking, if a large proportion of the literature supports something that matches with my own clinical experience, as well as the experience of my colleagues, then I don't have much reason to question it.
And ESP, Taps, pecs,etc are all fast and easy to perform blocks at our shop. Do paravertebrals and epidurals provide better analgesia? Sure. But they also require more expertise, higher risk, hypotension, require postop rounding, etc.
Should epidurals and PVB reimburse more? Absolutely
Should the lesser blocks also reimburse? Absolutely