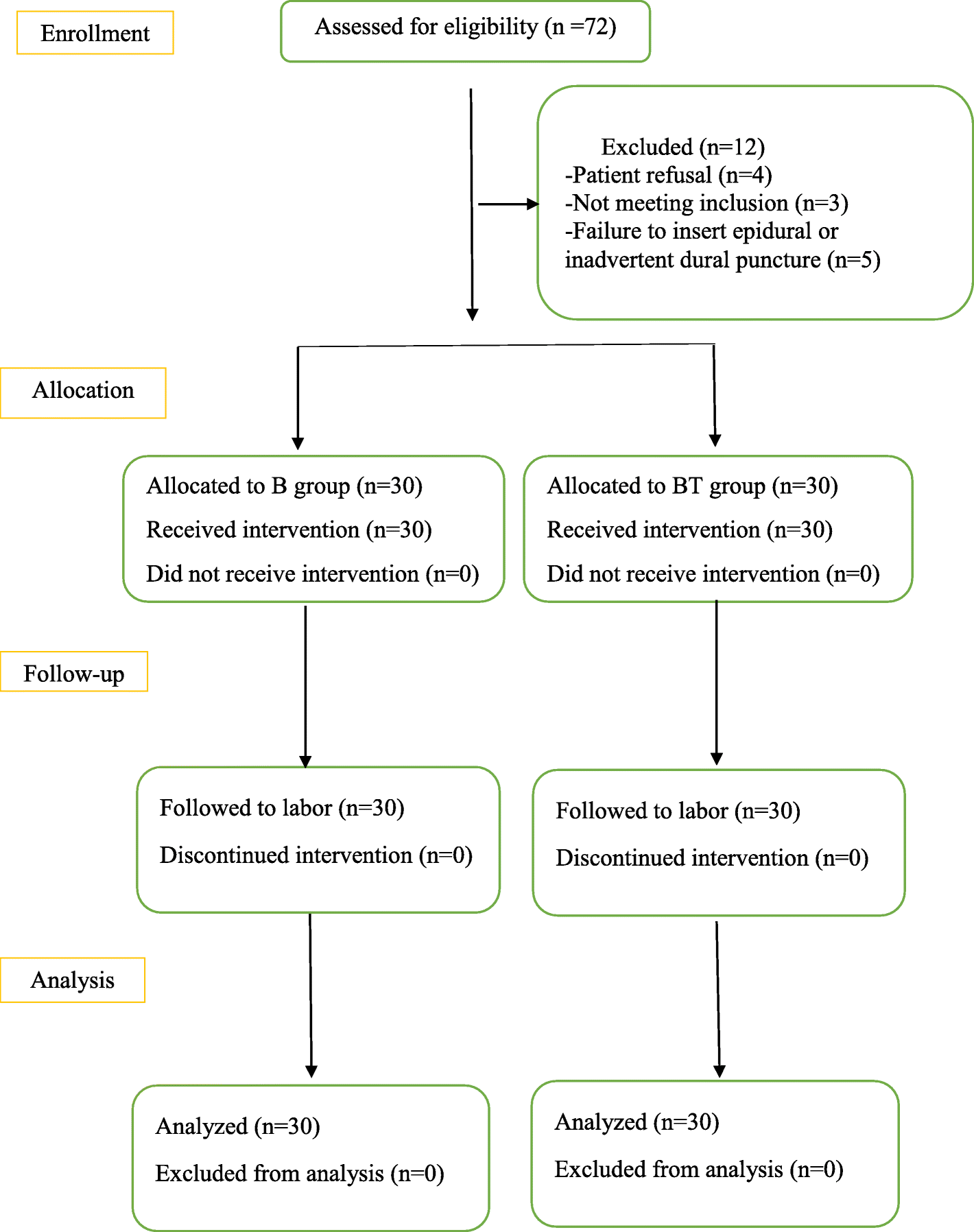
Background The efficacy and safety of spinal anesthesia by intrathecal dexmedetomidine (DEX) for parturients undergoing cesarean section are still lack of evidence. This aim of our study was to evaluate the efficacy and safety of intrathecal DEX for parturients undergoing cesarean section to...
bmcanesthesiol.biomedcentral.com
In our study, compared with intrathecal 9 mg of bupivacaine alone, the onset time of sensory and motor block of parturients in combination of 9 mg of intrathecal bupivacaine with 5 μg of DEX was significantly shortened, and the duration of sensory block was significantly prolonged by 40 min, which is consistent with the research results of Suthar’s [
20] and Sushruta’s [
10]. The mechanism may be as follows: DEX can activate the α-2 adrenergic receptor in the dorsal horn neurons, activate the spinal cord intermediate neurons by reducing the neurotransmitter released by the primary afferent end and G-protein-mediated potassium channel, and make the spinal cord intermediate neurons hyperpolarized, thus reducing the pain transmission. In addition, DEX can also block the internal flow of Na + and enhance the blocking effect of local anesthetics on the sodium channel of the cell membrane [
21,
22]. However, consisted with the results of a meta-analysis [
23] that included 9 RCTs, our study found that
motor block duration of paturients with intrathecal DEX was also prolonged, which suggest that combination with DEX may increase the fall risk and delay the early rehabilitation of parturients.