WOW! This thread got busy.. I really appreciate the relevant comments to my issue. first may I politely reply to this..
Ezekiel2517 said:
sorry to hear about the sore throat, but it's not from the LMA. The symptoms you're having 3 months after the surgery are not attributable to an LMA. There's a reason there probably isn't even a single case report describing a situation like yours 3 months out. It's bc it's not because of an LMA but from something else.
Please accept this respectfully. I mean no disrespect.
Having worked as a trouble shooter of highly technical plant machinery and an electrical engineer, for some 40 years, Once I learned that I knew enough to know I did not know anything in the larger picture, I quit making statements like that.
Read this article , Notice=
9 Months before full recovery I have included an excerpt quoted below.
http://journals.lww.com/anesthesia-...oid_Cartilage_Dislocation_Caused_by_a.37.aspx
IARS said:
Case Report
A 57-year-old, 70-kg, 155-cm woman, ASA physical status I, underwent right total knee replacement under general anesthesia at another institution. Her airway was managed uneventfully with a LMA. While insertion was noted to be without difficulty on one attempt, the size of the LMA used was not recorded. The duration of the procedure was 50 min.
The patient noticed hoarseness immediately postoperatively and sought consultation 4 wk later. Examination at that time by fiberoptic laryngoscopy showed an anteromedial dislocation of the right arytenoid cartilage with a flaccid and bowed vocal cord.
Six weeks postoperatively, the patient returned to the operating room for reduction and chemical splinting of the right arytenoid cartilage. This was performed under general anesthesia using intravenous propofol for induction and maintenance supplemented with fentanyl and succinylcholine for muscle relaxation. The airway was managed with infraglottic jet ventilation. After arytenoid reduction a total of 7.5 U of botulinum toxin was injected into the right thyroarytenoid and lateral cricoarytenoid muscles. The patient's hoarseness resolved within 4 wk postoperatively, and she was symptom free 9 mo later with normal arytenoid position and mobility.
I just read, I know nothing about this.
Ezekiel2517 said:
There's a reason there probably isn't even a single case report describing a situation like yours 3 months out.
Really ??
You probably should read this also
http://anesthesiology.pubs.asahq.org/article.aspx?articleid=2027840
The Journal of the American Society of Anesthesiologists said:
Case 2
A 54-yr-old woman, weighing 52 kg, underwent a dilatation and curettage and a breast biopsy. Preoperative assessment did not disclose any relevant medical history. After induction with 100 micro gram fentanyl and 3 mg [center dot] kg-1propofol, a fully deflated, size 3 LMA, lubricated with silicone spray, was easily inserted. The cuff was inflated with 30 ml air. Anesthesia was maintained with propofol, and the patient spontaneously breathed 60% N2O in oxygen. The procedure lasted 60 min. During recovery, the LMA was gently expelled by the patient. A few hours later, the patient complained of sore throat and dysphagia. The next day, hoarseness occurred. On the third day, the patient was aphonic and exhibited severe dysphagia, with laryngeal incompetence. A direct laryngoscopy showed an immobilized right vocal cord. The electromyogram confirmed a right recurrent nerve palsy. Dysphagia lasted 4 months, and dysphonia lasted 6 months. Six months after surgery, a stroboscopic examination showed partial recovery of vocal cord mobility.
Ezekiel2517 said:
And without knowing all the details, we can't tell you exactly what the cause is.
Now your talking sense.. 
(Nerve damage and cartilage damage have indeed been reported according to links some of you all have provided. ) (All I know is what I am reading )
As I said I did not come here to get doctored but I really appreciate the input. I came here to try to be informed before seeing a doctor. I read a lot and watched several videos of LMA insertion and removal including articles provided in links by FFP and others on this forum. Not to argue with them but to understand what they are telling me.
My appointment with the ENT last Wednesday did not go well. I chose the one of three in the firm because of her experience , years in the discipline.
Right out the gate when I said my voice sounded hoarse and I had a sore throat, She argued with me. That neither was true.. Ok trying to be a "Patient" patient and defer to her expertise, I explained that I "wondered" if there was a possibility that my issue was caused by either insertion, / over inflation / or improper removal of the LMA. (Admittedly I know nothing about this )
I was a bit put back when she insisted over and over that there was
"ENT" said:
nothing to deflate - inflate and there is no "Cuff" in an LMA.
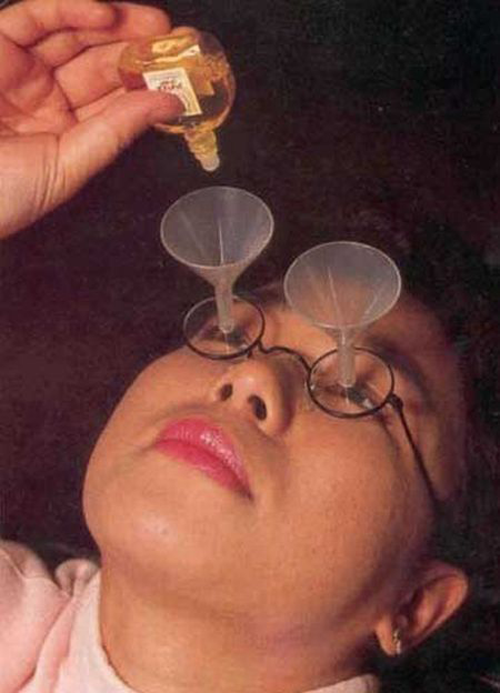
She spent - maybe 15 seconds looking down my throat through some round disc with a hole in the center positioned in front of her face and held there by a head band ( Yes, A head Mirror) I thought those were gone in the last century ... ( I have no problem with it, I suppose it is still a useful tool )
That was the entire exam. Your fine, ... have a good day............
Well I was glad she did not see anything obvious but I determined I would seek another ENT for another opinion, I am not a hypochondriac, My throat does indeed hurt and people do notice my horse voice.
My wife and I decided to explore other possibilities before making another appointment. I don't doctor myself, but I think my wife and I found out what is causing the problem.
We started looking at the side affects of the meds I was taking ( not that many really) Lipitor, Muscle relaxant, Oxycodine - generic for Percoset... as needed for pain.
Voila -- Sore throat and Horse voice both clearly listed as side affects for Percoset. I have been on it since the surgery.
I have noticed that the problem is more severe and noticeable at varying times (
maybe depending on frequency of dosage), I will monitor it more closely in relation to when I take the pain reliever.
It seems, after all the forms we fill out including telling doctors what meds we are taking, (Do they read this stuff? ) This could have and should have been diagnosed as a possible cause a long time ago by a doctor, not an electrical engineer and his accountant wife.
Thanks all of you. Very Much!