- Joined
- Apr 3, 2019
- Messages
- 4,274
- Reaction score
- 9,993
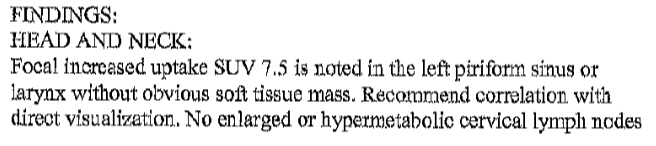
80yo male with history of controlled a-fib presents with BRBPR in Aug 2021 so bad he "almost passed out." H and H 11 and 31. Colonoscopy 9/21 shows 5cm cecal mass. 10/21, hemicolectomy specimen shows pT3 4cm mass, margins all negative, MSI-, 0/24 LNs positive. He is sent to med onc for eval. Med onc orders a pet scan on Oct 27.
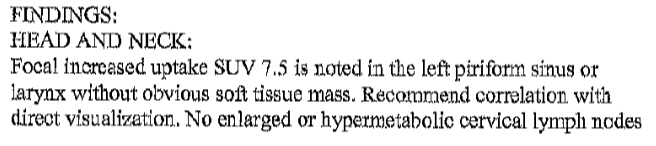
He is sent to ENT. ENT scopes him, sees nothing. Takes him to OR for directed biopsies of L pyriform sinus.
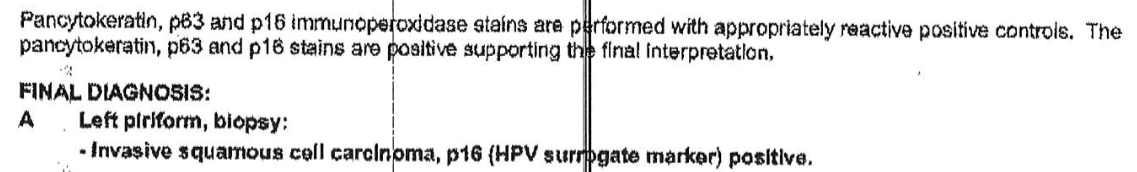
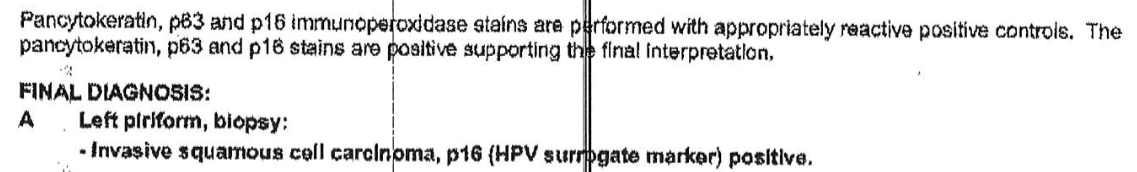
Four 0.2 to 0.7cm tissue specimens show
The patient is asymptomatic in the H&N region. And as mentioned clinical exam is negative.
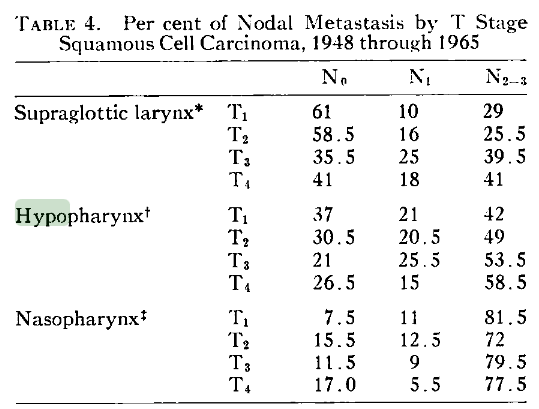
A T1N0 p16+ HNSCC of pyriform is a very rare clinical entity. Especially in an 80yo with recently diagnosed pT3N0 colon Ca.
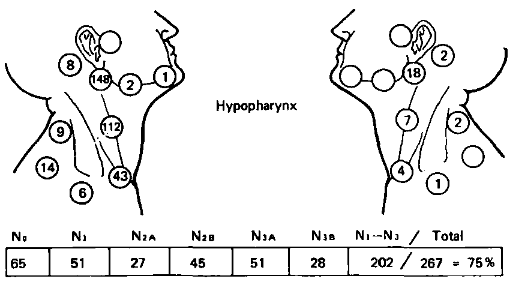
Wondering about XRT dose de-escalation, chemo, ENI to both necks, etc. My first thoughts are 60 Gy with low dose weekly CDDP to the L pyriform region, 45 Gy as the ENI dose to both necks.
He is sent to ENT. ENT scopes him, sees nothing. Takes him to OR for directed biopsies of L pyriform sinus.
Four 0.2 to 0.7cm tissue specimens show
The patient is asymptomatic in the H&N region. And as mentioned clinical exam is negative.
A T1N0 p16+ HNSCC of pyriform is a very rare clinical entity. Especially in an 80yo with recently diagnosed pT3N0 colon Ca.
Wondering about XRT dose de-escalation, chemo, ENI to both necks, etc. My first thoughts are 60 Gy with low dose weekly CDDP to the L pyriform region, 45 Gy as the ENI dose to both necks.