- Joined
- Nov 18, 2011
- Messages
- 330
- Reaction score
- 565
I've been sitting on this case for awhile, but it's a good one and I thought you all may be interested. I admitted this patient to the ICU from the ED. Let's roll:
HPI:-
Mid 50s patient presents to small ED complaining of shortness of breath. History of HTN, T2DM, Hypothyroidism. Recent tibia/fibula fracture s/p ORIF. Of note the patient had to be readmitted to the hospital for intractable pain and spent 4 days inpatient until an effective pain regimen was obtained. At that time compartment syndrome was ruled out. They are now presenting 3 days after discharge with worsening shortness of breath and per spouse, alteration of mental status.
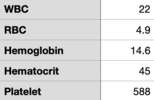
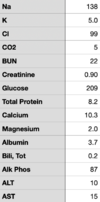
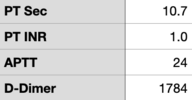
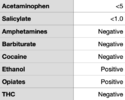
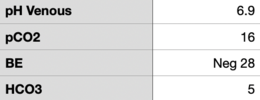
Small ED notes the patient had tachycardia, tachypnea and somnolence. CT scanner is down and no ability for VQ. After discussion with mothership ED they initiate an ED ➔ ED transfer. Patient arrives in mothership ED with the following vitals, labs obtained in the ED are found in the images I've attached.
Temp: 98.4 F
HR: 128
BP: 99/61 (MAP 73)
RR: 28
O2: 97% on 2L nasal cannula
Physical Exam as performed & documented by ED physician:
HENT: PERRL, moist mucous membranes
CV: tachycardia, regular rhythm, no m/g/r
Pulm: CTAB, tachypnea
Abd: Obese, soft, no tenderness
Neuro: GCS 8 (E2 V2 M4)
Extrem: No edema, 2+ peripheral pulses
More Patient History (obtained from spouse):
- Medical history as above
- Surgical history as above, +lap cholecystectomy (8 years prior)
- Current Everyday smoker, 1ppd x30 years
- occasional EtOH
Med List (spouse brought it in!)
- Aspirin 81mg daily
- Methocarbamol
- Dulaglutide
- Venlafaxine
- Empaglifozin
- D3
- Rosuvastatin
- Pantoprazole
- Metformin
- Lisinopril
- Glipizide
ED physician obtained a CT PE. There was significant motion artifact, but no clear PE in the Left/Right main pulmonary artery, segmental likely clear. Subsegmental cannot be evaluated.
At this point the patient was admitted to the ICU with diagnosis of respiratory failure, possibly PE. A DVT study was ordered by ED but not completed prior to transfer. So this is what I know when the patient comes to the ICU. Think about what your differential is for this patient, what other workup you think you'd want. I'll start post #2 now, so more info coming.
HPI:-
Mid 50s patient presents to small ED complaining of shortness of breath. History of HTN, T2DM, Hypothyroidism. Recent tibia/fibula fracture s/p ORIF. Of note the patient had to be readmitted to the hospital for intractable pain and spent 4 days inpatient until an effective pain regimen was obtained. At that time compartment syndrome was ruled out. They are now presenting 3 days after discharge with worsening shortness of breath and per spouse, alteration of mental status.
Small ED notes the patient had tachycardia, tachypnea and somnolence. CT scanner is down and no ability for VQ. After discussion with mothership ED they initiate an ED ➔ ED transfer. Patient arrives in mothership ED with the following vitals, labs obtained in the ED are found in the images I've attached.
Temp: 98.4 F
HR: 128
BP: 99/61 (MAP 73)
RR: 28
O2: 97% on 2L nasal cannula
Physical Exam as performed & documented by ED physician:
HENT: PERRL, moist mucous membranes
CV: tachycardia, regular rhythm, no m/g/r
Pulm: CTAB, tachypnea
Abd: Obese, soft, no tenderness
Neuro: GCS 8 (E2 V2 M4)
Extrem: No edema, 2+ peripheral pulses
More Patient History (obtained from spouse):
- Medical history as above
- Surgical history as above, +lap cholecystectomy (8 years prior)
- Current Everyday smoker, 1ppd x30 years
- occasional EtOH
Med List (spouse brought it in!)
- Aspirin 81mg daily
- Methocarbamol
- Dulaglutide
- Venlafaxine
- Empaglifozin
- D3
- Rosuvastatin
- Pantoprazole
- Metformin
- Lisinopril
- Glipizide
ED physician obtained a CT PE. There was significant motion artifact, but no clear PE in the Left/Right main pulmonary artery, segmental likely clear. Subsegmental cannot be evaluated.
At this point the patient was admitted to the ICU with diagnosis of respiratory failure, possibly PE. A DVT study was ordered by ED but not completed prior to transfer. So this is what I know when the patient comes to the ICU. Think about what your differential is for this patient, what other workup you think you'd want. I'll start post #2 now, so more info coming.
Attachments
Last edited: