- Joined
- Oct 4, 2017
- Messages
- 5,029
- Reaction score
- 9,816
Looking at editors choice, while in a really bad mood, but think legitimate points here.
New Editor's Choice citations and comments have been filed in your ACR Journal Advisor Radiation Oncology library.
This month's titles include:
New Editor's Choice citations and comments have been filed in your ACR Journal Advisor Radiation Oncology library.
This month's titles include:
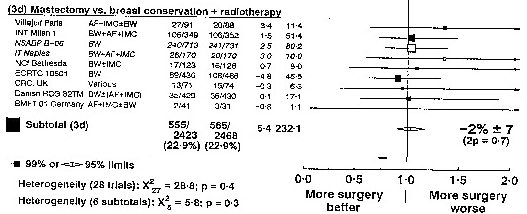
- Breast: Refined estimates of local recurrence risks by DCIS score adjusting for clinicopathological features: a combined analysis of ECOG-ACRIN E5194 and Ontario DCIS cohort studies. Great, can we eliminate xrt? Unless comedo, high grade dcis or young pt, we know xrt is optional in this setting.
- Breast: A biological signature for breast ductal carcinoma in situ to predict radiotherapy benefit and assess recurrence risk
- can we eliminate xrt?
- Central Nervous System: Updates in the management of intradural spinal cord tumors: a radiation oncology focus.
- Gastrointestinal: Tumour regression after radiotherapy for rectal cancer - Results from the randomised Stockholm III trial.
- Head and Neck / Skin: Effect of Doxepin Mouthwash or Diphenhydramine-Lidocaine-Antacid Mouthwash vs Placebo on Radiotherapy-Related Oral Mucositis Pain: The Alliance A221304 Randomized Clinical Trial.
- Health Services Research: Variations in Medicaid Payment Rates for Radiation Oncology
- medicaid suck unless you are in a handful of states
- Lung and Mediastinum: Local Consolidative Therapy Vs. Maintenance Therapy or Observation for Patients With Oligometastatic Non-Small-Cell Lung Cancer: Long-Term Results of a Multi-Institutional, Phase II, Randomized Study.
- Pediatrics: Curative-intent radiotherapy for pediatric osteosarcoma: The St. Jude experience.
- Dont give a XXXX. All you need to know is to send it to St Jude if you see one. (they fund flying out the patient and their family,) 99% of radoncs should not attempt to treat most pediatric malignancies.
- Soft Tissue Sarcoma: Radiotherapy for Retroperitoneal Liposarcoma: A Report From the Transatlantic Retroperitoneal Sarcoma Working Group
Last edited: