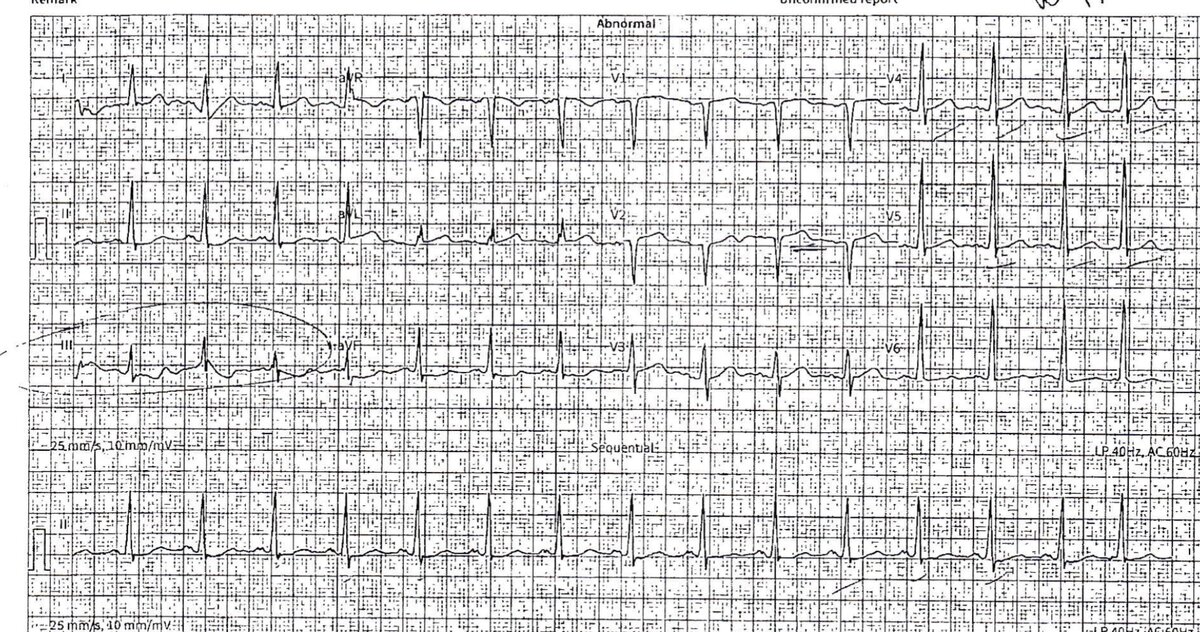
Maybe im susceptible to peer pressure (first few comments on this thread) but honestly if you handed me the ekg on shift instead of with the idea that “looked like a missed stemi to my colleagues” I think I would probably say changes in iii were artifact, ii might be actual st depression, and don’t appreciate anything in v1 and minimal in v2.
in a chest pain pt I would call because if the cards guy at my place doesn’t want to keep them I need to know.
in this patient?
if a nervous colleague asked me about it I’d tell them to call cards so they could sleep that night and not think about it. If I was feeling crushed or having decision fatigue I would probably call cards so I could stop thinking about it. When I’m in doubt, I usually call the person who will be judging me later.
My threshold for calling for reassurance increases significantly at 5p and 10p-7a though out of respect for colleagues circadian rhythms. But we all sometimes make stupid consults, same as consultants turf to us for stupid office stuff sometimes.
I can respect that. I made a thread a few weeks ago about how as a new attending I feel like a wuss, have a tendency to over consult, over admit etc.
My algorithm for these cases is very simple.
1. STEMI criteria met: call cards/activate cath lab. This EKG, I think we can agree, that maybe has some abnormalities but does not warrant cath lab activation.
2. Evolving MI: dynamic EKG changes, rising trops, persistent chest pain, I call cards. Maybe he will be a "sooner than later" cath.
3. Positive trops, maybe non specific EKG changes, but patient otherwise stable: meh. The inpatient team can call cards in the morning. They will just trend it out and monitor on tele. This patient is not getting an emergent cath regardless, so makes no sense to call emergently IMO.
4. Everything else: don't call cards, ensure good outpatient follow up if discharging, otherwise punt to inpatient team.
I'd say if I'm going to discharge a patient and want someone to take a second look at the EKG, it's not unreasonable, especially so I can get some sleep at night. But if I am squinting really hard at an EKG and convincing myself about a little elevation here, or a little elevation there, chances are I am psyching myself out, and I will continue to get a few more EKGs/trops which will further support my notion that the person is not having a significant MI.
The patient in the original post is getting admitted, so... I probably wouldn't lose any sleep over this one.