yoloswagpoop42069
Full Member
- Joined
- Sep 28, 2022
- Messages
- 95
- Reaction score
- 68
Gearing up for my first job outside residency at an addiction recovery center (outpatient clinic)
Sad to say, residency training has not given me the volume of outpatient Suboxone patients to feel comfortable with all the details of Suboxone induction.
Looking online, there are a variety of Suboxone initiation protocols available, with variable dosing schedules.
Since I'm just getting started, I would like a concrete protocol to operate on for the first month, and then be more flexible and tailor it from there. All Suboxone initiations at the outpatient clinic will be home inductions (so no office-based induction/watching first dose).
What is your go-to Suboxone initiation prescribing protocols for reliable, health-literate patients, after the usual assessment/psychoeducation is provided?
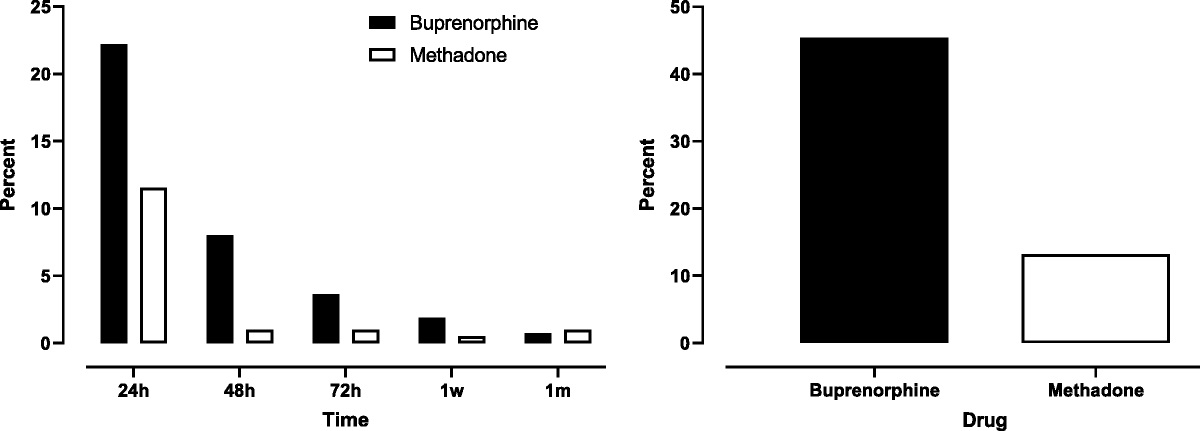
From this ASAM guide it suggests flexible home dosing on Days 1-3:
But using this, I believe it then necessitates follow-up on Day 4 to address maintenance dosing?
And if using this protocol, I get confused on how many 4 mg tablets/strips I should prescribe so they are covered for the flexibility?
This Yale guide, based on ED-visit initiations, is way more concrete:
With Day 1 dosing of three 4 mg strips for a total of 12 mg on Day 1
And then straight up 16 mg from Days 2-7
With follow-up 1 week later.
Right now, I am thinking about following the Yale ED protocol as it's more concrete, and I know exactly how many tabs/strips I need to prescribe, and allows for concrete follow-up in 1 week to assess maintenance dose. But since it goes quickly to 16 mg per day, I wonder about the patients who do not need so much, and perhaps need only 8 mg Daily, although I assume the majority of patients will need at least 16 mg, so maybe I can flex this protocol to 8 mg daily for those who are not using much per day, but still want Suboxone.
@SubzDoc or anyone else who routinely initiates Suboxone, your guidance in this would be appreciated.
Sad to say, residency training has not given me the volume of outpatient Suboxone patients to feel comfortable with all the details of Suboxone induction.
Looking online, there are a variety of Suboxone initiation protocols available, with variable dosing schedules.
Since I'm just getting started, I would like a concrete protocol to operate on for the first month, and then be more flexible and tailor it from there. All Suboxone initiations at the outpatient clinic will be home inductions (so no office-based induction/watching first dose).
What is your go-to Suboxone initiation prescribing protocols for reliable, health-literate patients, after the usual assessment/psychoeducation is provided?
From this ASAM guide it suggests flexible home dosing on Days 1-3:
But using this, I believe it then necessitates follow-up on Day 4 to address maintenance dosing?
And if using this protocol, I get confused on how many 4 mg tablets/strips I should prescribe so they are covered for the flexibility?
This Yale guide, based on ED-visit initiations, is way more concrete:
With Day 1 dosing of three 4 mg strips for a total of 12 mg on Day 1
And then straight up 16 mg from Days 2-7
With follow-up 1 week later.
Right now, I am thinking about following the Yale ED protocol as it's more concrete, and I know exactly how many tabs/strips I need to prescribe, and allows for concrete follow-up in 1 week to assess maintenance dose. But since it goes quickly to 16 mg per day, I wonder about the patients who do not need so much, and perhaps need only 8 mg Daily, although I assume the majority of patients will need at least 16 mg, so maybe I can flex this protocol to 8 mg daily for those who are not using much per day, but still want Suboxone.
@SubzDoc or anyone else who routinely initiates Suboxone, your guidance in this would be appreciated.