inspired by a long thoughtful conversation with a PACU nurse I had this week about changing patterns in regional anesthesia, I'm wondering about practice patterns with nerve stimulators these days for blocks done under ultrasound guidance. Specifically things like an interscalene block or popliteal block where it could be done either with pure ultrasound or pure nerve stimulator technique or a combination of both. Obviously I assume nobody is using a nerve stimulator for something like a plane block.
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Survey on use of nerve stimulators in regional anesthesia
- Thread starter Mman
- Start date
- Joined
- Sep 27, 2017
- Messages
- 693
- Reaction score
- 1,442
I use it once in a while if the picture doesn't look perfect and I want to confirm I'm injecting by nerve and not some random structure
D
deleted875186
Never even learned how to use it in residency
Arch Guillotti
Senior Member
Staff member
Administrator
Volunteer Staff
Lifetime Donor
20+ Year Member
- Joined
- Aug 9, 2001
- Messages
- 9,566
- Reaction score
- 6,455
sameI use it once in a while if the picture doesn't look perfect and I want to confirm I'm injecting by nerve and not some random structure
- Joined
- Jan 14, 2006
- Messages
- 11,882
- Reaction score
- 20,913
Never even learned how to use it in residency
Nerve stimulator, paresthesia, and transarterial was all we had in residency but I never use any of those techniques any more.
- Joined
- Nov 12, 2015
- Messages
- 308
- Reaction score
- 691
I use it, along with ultrasound. It's how I trained. My goal is not necessarily to demonstrate stim, it's to ensure I'm not injecting at a low threshold (like < 0.3mA). In my mind, it's just a small, simple way to reduce the risk of nerve injury. No shame to those who don't use it -- I get it.
- Joined
- Jan 13, 2016
- Messages
- 195
- Reaction score
- 226
3 times during residency
- Joined
- Apr 15, 2020
- Messages
- 26
- Reaction score
- 78
I do occasionally use stim to confirm that I'm getting the musculocutaneous nerve during an axillary block, since it's not always obvious. That's about it.
I do occasionally use stim to confirm that I'm getting the musculocutaneous nerve during an axillary block, since it's not always obvious. That's about it.
If you scan up into the axilla and then distally it’s usually pretty obvious.
Arch Guillotti
Senior Member
Staff member
Administrator
Volunteer Staff
Lifetime Donor
20+ Year Member
- Joined
- Aug 9, 2001
- Messages
- 9,566
- Reaction score
- 6,455
usually. not alwaysIf you scan up into the axilla and then distally it’s usually pretty obvious.
usually. not always
If your ultrasound is decent quality you should be able to identify it pretty easily. I do axillary blocks fairly regularly and I’ve never needed a nerve stimulator to identify MCN.
- Joined
- Apr 15, 2020
- Messages
- 26
- Reaction score
- 78
If your ultrasound is decent quality you should be able to identify it pretty easily. I do axillary blocks fairly regularly and I’ve never needed a nerve stimulator to identify MCN.
The axillary block is my least utilized upper extremity block, I do very few. I agree that usually the MCN is visible, but for a block I barely use I have a crutch (the stim) on standby so I can be sure to get it if I have any doubts.
D
deleted1111114
I do for every applicable block because surgeon’s lawyers will send out the same poll to every “expert”. I think one of the block associations recommends using both now as a guideline - could be wrong.
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
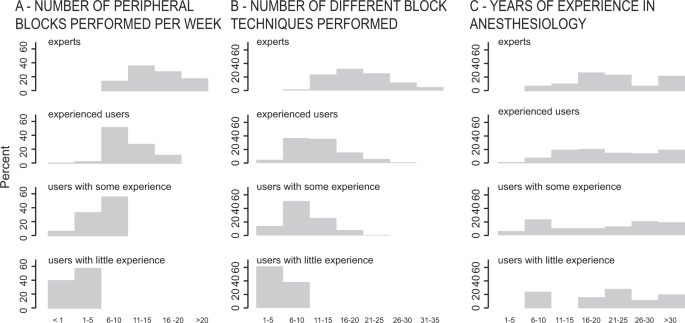
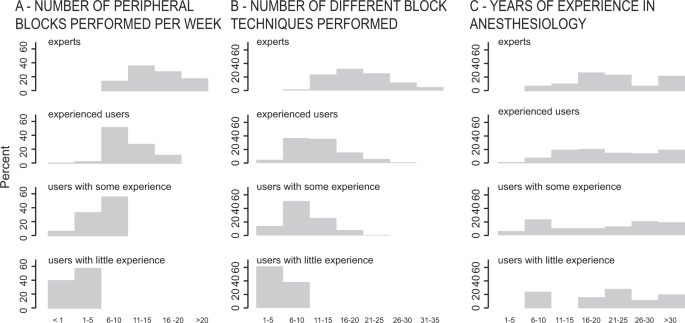
The use of electrical nerve stimulation in combination with ultrasound guidance has been recommended to reduce the risk of intraneural needle placement6,7,8. Less than half of the anesthesiologists participating in the survey used ultrasound as a sole technique in most cases. While some authors recommended a minimal current threshold of 0.5 mA for electrical nerve stimulation, others considered using thresholds as high as 0.8–1.0 mA to avoid traumatic needle-to-nerve contact9,10,11. The minimal current thresholds used by the survey participants were often lower than recommended. The German guidelines regarding nerve localization for peripheral nerve blocks state that low threshold currents (<0.5 mA) may potentially increase unintentional intraneural needle placement12.
 www.nature.com
www.nature.com
A Swiss nationwide survey shows that dual guidance is the preferred approach for peripheral nerve blocks - Scientific Reports
Ultrasound has significantly increased safety and effectiveness in regional anesthesia. However, little is known about its clinical use. We studied clinical approaches currently used by anesthesiologists, conducted a nationwide survey, and analyzed data collected in ordered logistic regression...
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
In principle, almost all plexuses or other large peripheral nerves can be located using PNS. When used with ultrasound guidance, PNS becomes primarily a safety tool. The goal of nerve stimulation is to place the tip of the needle (more specifically, its orifice for injection) in close proximity to the target nerve to inject the local anesthetic within the tissue space that contains the nerve. When used with ultrasound guidance, PNS becomes primarily a safety tool. An unexpected motor response during needle advancement may alert the operator that the needle is in immediate vicinity to the nerve and therefore, prevent further needle advancement when the needle tip position is not well seen on ultrasound. The motor response (twitch) to PNS is objective, reliable and independent from the patient’s (subjective) response. Even with ultrasound guidance, nerve stimulation is often helpful to confirm that the structure imaged is actually the nerve that is sought. Likewise, the needle-nerve relationship may not always be visualized on ultrasound; an unexpected motor response can occur, alerting the operator that the needle is already in close proximity to the nerve. The occurrence of a motor response at a current intensity of less than 0.5 mA can serve as an indicator of a needle-nerve contact or intraneural needle placement. Although this response may not be present even with an intraneural needle position (low sensitivity), its presence is essentially always indicative of intraneural placement (high specificity)

 www.nysora.com
www.nysora.com

Electrical Nerve Stimulators and Localization of Peripheral Nerves - NYSORA
Peripheral nerve stimulation (PNS), an important tool to aid administration of peripheral nerve blocks. Improvements in electrical nerve localization technology have led to a number of commercially available nerve stimulators that are superior and more advanced compared to older devices. With...
I do for every applicable block because surgeon’s lawyers will send out the same poll to every “expert”. I think one of the block associations recommends using both now as a guideline - could be wrong.
I think it is mostly going by the wayside. I use one exceedingly rarely. I am a bit surprised it isn't even being taught to residents at this point in at least some places. Is there any actual evidence it improves safety?
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
Together, ultrasound and electronic nerve stimulation are complementary to each other and increase the likelihood that intraneural injections will be detected and prevented.
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
For instance, Retter et al. performed US-guided supraclavicular blocks on cadavers and histologically found a 24% incidence of sub-perineural injections. While such a high incidence of neurological complications or cadaveric structural integrity are not seen in clinical practice, their findings demonstrate that the lateral resolution of the US is not high enough to differentiate intra- and extrafascicular injections.[17] Furthermore, although subclinical, one cannot advocate for intraneural injection since LA deposition directly around nerve fascicles has been hypothesized to result in cytotoxicity and ischemia.[18,19,20] Such effects are seen in large animal histopathologic models and may be prevented by avoiding nerve perforation.[21] Overall, peripheral nerve injuries (PNIs) are complicated and multifactorial (see Table 1).
This finding supports the argument that more than one technique should be used to help prevent nerve injury when performing nerve block (dual-endpoint technique).
This finding supports the argument that more than one technique should be used to help prevent nerve injury when performing nerve block (dual-endpoint technique).
- Joined
- May 2, 2012
- Messages
- 2,516
- Reaction score
- 1,131
Not a great poll. I use a nerve stimulator (and ultrasound) for basically every interscalene block I do, because we do a ton of train wrecks and redo's that have significantly distorted anatomy. And even on our patients that aren't that, I've seen failed blocks that looked picture perfect on ultrasound. My own picture has looked perfect with no twitch, and when I advance a hair further I actually do pop through a small layer of fascia and that would have been the difference of me redoing the block post op.
With that said, there's no point in using one for say, an adductor canal block where it's almost pure sensory. So because of this I clicked "sometimes" on the poll even though with some blocks I "always" use it.
With that said, there's no point in using one for say, an adductor canal block where it's almost pure sensory. So because of this I clicked "sometimes" on the poll even though with some blocks I "always" use it.
For instance, Retter et al. performed US-guided supraclavicular blocks on cadavers and histologically found a 24% incidence of sub-perineural injections. While such a high incidence of neurological complications or cadaveric structural integrity are not seen in clinical practice, their findings demonstrate that the lateral resolution of the US is not high enough to differentiate intra- and extrafascicular injections.[17] Furthermore, although subclinical, one cannot advocate for intraneural injection since LA deposition directly around nerve fascicles has been hypothesized to result in cytotoxicity and ischemia.[18,19,20] Such effects are seen in large animal histopathologic models and may be prevented by avoiding nerve perforation.[21] Overall, peripheral nerve injuries (PNIs) are complicated and multifactorial (see Table 1).
This finding supports the argument that more than one technique should be used to help prevent nerve injury when performing nerve block (dual-endpoint technique).
the problem with cadaver studies is the only outcome we care about is permanent nerve injury and they provide no data about that
Arch Guillotti
Senior Member
Staff member
Administrator
Volunteer Staff
Lifetime Donor
20+ Year Member
- Joined
- Aug 9, 2001
- Messages
- 9,566
- Reaction score
- 6,455
Why is the anatomy distorted? Do you mean because of pt. positioning?Not a great poll. I use a nerve stimulator (and ultrasound) for basically every interscalene block I do, because we do a ton of train wrecks and redo's that have significantly distorted anatomy. And even on our patients that aren't that, I've seen failed blocks that looked picture perfect on ultrasound. My own picture has looked perfect with no twitch, and when I advance a hair further I actually do pop through a small layer of fascia and that would have been the difference of me redoing the block post op.
With that said, there's no point in using one for say, an adductor canal block where it's almost pure sensory. So because of this I clicked "sometimes" on the poll even though with some blocks I "always" use it.
- Joined
- May 2, 2012
- Messages
- 2,516
- Reaction score
- 1,131
Severe surgical changes, patient positioning as well. I just did an interscalene block on a guy last week that had a completely dislocated humeral head just hanging out. This was his 12th surgery. He had scar tissue all the way up his neck. I never saw the brachial plexus. Ultrasound was only useful to stay out of vessels and identify what possibly might be the scalene muscles. Nerve stimulator and a lot of luck led to a successful block.Why is the anatomy distorted? Do you mean because of pt. positioning?
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
Your problem of not using a nerve stimulator when performing certain blocks is when a complication occurs secondary to your block or the surgery. Since ASRA and many others recommend its use you will be more exposed to litigation by so-called experts that you didn't meet the standard of care. A jury will see the recommendation by ASRA and be more inclined to believe them than your so called expert.the problem with cadaver studies is the only outcome we care about is permanent nerve injury and they provide no data about that
Your problem of not using a nerve stimulator when performing certain blocks is when a complication occurs secondary to your block or the surgery. Since ASRA and many others recommend its use you will be more exposed to litigation by so-called experts that you didn't meet the standard of care. A jury will see the recommendation by ASRA and be more inclined to believe them than your so called expert.
I'm not asking about the legal ramifications which depends on which state you are in. There is a nearly unlimited supply of experts to testify it is not standard of care which is all that matters. I'm just pointing out there is no actual evidence it decreases complications.
also, I have never had a problem when I didn't use a nerve stimulator and I don't think I ever met someone that got successfully sued for a nerve injury attributed to not using a nerve stimulator.
Last edited:
Arch Guillotti
Senior Member
Staff member
Administrator
Volunteer Staff
Lifetime Donor
20+ Year Member
- Joined
- Aug 9, 2001
- Messages
- 9,566
- Reaction score
- 6,455
Your problem of not using a nerve stimulator when performing certain blocks is when a complication occurs secondary to your block or the surgery. Since ASRA and many others recommend its use you will be more exposed to litigation by so-called experts that you didn't meet the standard of care. A jury will see the recommendation by ASRA and be more inclined to believe them than your so called expert.



- Joined
- May 2, 2012
- Messages
- 2,516
- Reaction score
- 1,131
I cannot imagine you'd find many people that would state confidently that using a nerve stimulator is standard of care.
What if someone used a nerve stimulator without ultrasound and there was a bad outcome? I'd have to think ultrasound if available is closer to standard of care than nerve stimulators are. Coming from someone who uses a nerve stimulator any time I can.
What if someone used a nerve stimulator without ultrasound and there was a bad outcome? I'd have to think ultrasound if available is closer to standard of care than nerve stimulators are. Coming from someone who uses a nerve stimulator any time I can.
- Joined
- Jan 14, 2006
- Messages
- 11,882
- Reaction score
- 20,913
There’s no study showing that using both reduces the rate of nerve injury. It’s just an unproven conjecture. A lot of reasonable ideas don’t hold up under scrutiny.
D
deleted1111114
I cannot imagine you'd find many people that would state confidently that using a nerve stimulator is standard of care.
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
U/S increases the success of a block and decreases the amount of local needed vs a nerve stimulator only block. However, the safety of U/S vs Nerve Stimulator in terms of nerve related injuries has never been shown to be different. What we do know is that the combination of nerve stimulation with U/S increases both the safety and success of the block.I cannot imagine you'd find many people that would state confidently that using a nerve stimulator is standard of care.
What if someone used a nerve stimulator without ultrasound and there was a bad outcome? I'd have to think ultrasound if available is closer to standard of care than nerve stimulators are. Coming from someone who uses a nerve stimulator any time I can.
- Joined
- Jan 14, 2006
- Messages
- 11,882
- Reaction score
- 20,913
What we do know is that the combination of nerve stimulation with U/S increases both the safety and success of the block.
That would be game changing if true. Where has this been shown?
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
Conclusion
Despite countless studies attempting to outline differences in outcomes between US and ENS in regional anesthesia, neither technique is reliable on its own. Rather, when used together these modalities are complementary to each other and increase the likelihood that intraneural injections will be detected and prevented.[27]Conclusion
Despite countless studies attempting to outline differences in outcomes between US and ENS in regional anesthesia, neither technique is reliable on its own. Rather, when used together these modalities are complementary to each other and increase the likelihood that intraneural injections will be detected and prevented.[27]
that conclusion does not show any increase in safety, merely conjecture that it is safer which has never been shown
- Joined
- Feb 6, 2014
- Messages
- 393
- Reaction score
- 653
These nysora videos always give me a laugh. So detached from the reality of practice most of the time.
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
Sort of like the parachute analogy where they haven't been shown to be effective either. There is no reason not to hook up a nerve stimulator as an additional safety feature. The point behind the stimulator is to increase safety not to facilitate the block. I know this adds about a minute to the procedure time but the additional safety factor with its use makes the 1 minute worth it IMHO.that conclusion does not show any increase in safety, merely conjecture that it is safer which has never been shown
Sort of like the parachute analogy where they haven't been shown to be effective either. There is no reason not to hook up a nerve stimulator as an additional safety feature. The point behind the stimulator is to increase safety not to facilitate the block. I know this adds about a minute to the procedure time but the additional safety factor with its use makes the 1 minute worth it IMHO.
unlike the parachute analogy, we probably have millions of blocks done without a nerve stimulator showing them to be safe and there is no evidence I have ever seen showing it to improve safety by using a nerve stimulator.
Last edited:
- Joined
- Feb 13, 2011
- Messages
- 477
- Reaction score
- 578
that conclusion does not show any increase in safety, merely conjecture that it is safer which has never been shown
Sort of like the parachute analogy where they haven't been shown to be effective either. There is no reason not to hook up a nerve stimulator as an additional safety feature. The point behind the stimulator is to increase safety not to facilitate the block. I know this adds about a minute to the procedure time but the additional safety factor with its use makes the 1 minute worth it IMHO.
Right, even the NYSORA video stretches to make conclusions and real world practicality of improved safety.
Injection pressure of 50 psi (!!!) will detect 95% of intraneural injections.
They mention that only a tiny amount of local anesthetic (without quantifying a volume) can be damaging, thus ultrasound isn’t any more safe than not using it specific to intraneural injections. They say US helps with LAST they say but not intraneural.
And they recommend keeping the nerve stimulator on for the duration of the procedure to 0.5 (cause COVID to have less people near by so it can set and forget instead of a sole nerve stimulator operator). So the patient is uncomfortable before I’m ready to inject and they twitch as I’m moving past something but not injecting? That plan doesn’t make sense to me. And the marker is 0.3 not 0.5
But somehow using all 3 help? Sounds like the falicy of meta analysis if the underlying data isn’t great.
- Joined
- Apr 22, 2007
- Messages
- 22,315
- Reaction score
- 8,964
I perform Nerve stimulator with U/S blocks routinely. I set the stimulator to 0.5 and perform the block. If I get a twitch (1 twitch every 2 seconds) I simply move the needle away from the nerve. This takes about 3-5 seconds. The only time that a small distance may affect neve block success is with the popliteal block where there is a paraneural sheath which requires close injection. But, most of the time you won't get a twitch with a popliteal block at 0.5 anyway just by being in proximity to the nerve.Right, even the NYSORA video stretches to make conclusions and real world practicality of improved safety.
Injection pressure of 50 psi (!!!) will detect 95% of intraneural injections.
They mention that only a tiny amount of local anesthetic (without quantifying a volume) can be damaging, thus ultrasound isn’t any more safe than not using it specific to intraneural injections. They say US helps with LAST they say but not intraneural.
And they recommend keeping the nerve stimulator on for the duration of the procedure to 0.5 (cause COVID to have less people near by so it can set and forget instead of a sole nerve stimulator operator). So the patient is uncomfortable before I’m ready to inject and they twitch as I’m moving past something but not injecting? That plan doesn’t make sense to me. And the marker is 0.3 not 0.5
But somehow using all 3 help? Sounds like the falicy of meta analysis if the underlying data isn’t great.
- Joined
- Apr 24, 2012
- Messages
- 4,470
- Reaction score
- 4,997
Regional guy at my residency program would use stim at 0.3 just to protect the nerve. If you get any twitch, you're too close and need to pull back until you lost the twitch, then inject. Makes sense to me. Ultrasound to find the nerve, stim to avoid intraneural. Especially helpful with trainees. And this is just for big motor nerves. Adductor canal? No stim needed.
- Joined
- Jan 19, 2011
- Messages
- 211
- Reaction score
- 64
All this discussion is great. I only wonder if a jury would see the nuance.
A lot of you have never been sued, and it shows. Protect yourself.
A lot of you have never been sued, and it shows. Protect yourself.
All this discussion is great. I only wonder if a jury would see the nuance.
A lot of you have never been sued, and it shows. Protect yourself.
I have never even heard of a successful lawsuit related to lack of nerve stimulator use. I mean I am sure it is out there somewhere, but it's the sort of thing you are unlikely to experience in your career.
And if you have a permanent nerve injury related to a nerve block it is quite unlikely that documented stimulator use is going to change the outcome of the lawsuit.
- Joined
- Nov 12, 2015
- Messages
- 308
- Reaction score
- 691
I agree that stimulator usage would not change the outcome of a lawsuit for a peripheral nerve injury. I’m just banking on it keeping me out of trouble in the first place. I don’t inject on low thresholds; meanwhile my partners don’t mind seeing stim at < 0.2mA.I have never even heard of a successful lawsuit related to lack of nerve stimulator use. I mean I am sure it is out there somewhere, but it's the sort of thing you are unlikely to experience in your career.
And if you have a permanent nerve injury related to a nerve block it is quite unlikely that documented stimulator use is going to change the outcome of the lawsuit.
- Joined
- Sep 19, 2018
- Messages
- 738
- Reaction score
- 532
Personally have seen it and assisted others only unfortunately.
3 years ago, Pajunk had a local representative in Iraq - not anymore and an Anesthesiologist bought dozens of those PNSs and sold them to other, it was affordable like 500 USD - I am not sure if that a good price.
I know a resident over here who did hundreds of blocks using only PNS. It is very useful if you practice with it. I intend to buy a portable US and PNS for myself once I get out safely from the Board.
3 years ago, Pajunk had a local representative in Iraq - not anymore and an Anesthesiologist bought dozens of those PNSs and sold them to other, it was affordable like 500 USD - I am not sure if that a good price.
I know a resident over here who did hundreds of blocks using only PNS. It is very useful if you practice with it. I intend to buy a portable US and PNS for myself once I get out safely from the Board.
- Joined
- Sep 19, 2018
- Messages
- 738
- Reaction score
- 532
This is very interesting Dr.
Do you have similar scheme for major blocks effect of PNS to get it as a reference for the future.
Similar threads
- Replies
- 10
- Views
- 2K
