2
24858
Spinal vs general. Thoughts?
What's profound? 124? Or 114? Or 104?Spinal vs general. Thoughts?
Lets go with 115-120 range, what would be your preferred method of anesthesia and why?
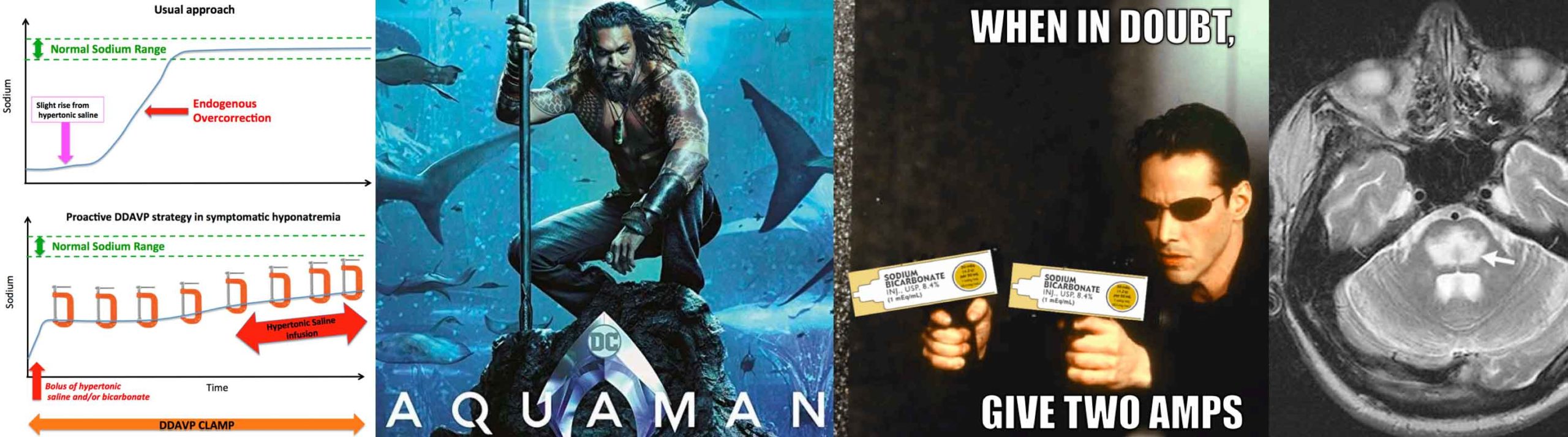
That’s profound. I need her asleep and I need to be pushing some Sodium Bicarb first if less than <110. I mean she could be getting to seizure zone from Cerebral Edema. What’s her GCS neuro exam? Is this because of Preeclampsia and water retention?Lets go with 115-120 range, what would be your preferred method of anesthesia and why?
I was curious whether a spinal would be contraindicated in profound hyponatremia due to possible cerebral edema.
because it has a higher concentration of sodium than hypertonic salinewhy would you used bicarb?
Interesting thank you. Would you then be concerned with myelinolysis?
Depends on how severe, and how acute And the OP is being vague about that fact.honestly, this sounds subacute and incidental, if that’s truly the case then I don’t think I’d go trying to correct the Na while also doing a c section. Both will have dramatic effects on volume and solute status making correction in this moment extremely difficult and unpredictable. LR is what I use 99% of the time and is why I would continue to use it in this situation. The worse thing you can do in this situation is over correct.
I'm thinking spinal if normal mental status. LR for fluids. With a sodium content of 130mEq in the LR, I'm not worried that I'm going to correct too quickly with the usual 1-2L LR given during a C/S.Spinal vs general. Thoughts?
NS is 154mEq of both Na+ and Cl-.Assuming this has to go now and patient has normal GCS would proceed with spinal. Would use LR as fluid of choice since it’s Na of 130 (relative to normal saline’s Na of 145) is less likely to dangerously overcorrect and cause osmotic demyelination. Would lean more on pressors than fluid as other have stated for same reasons. If patient seizes or has acute change in mental status that isn’t responsive to neo/ephedrine I’ll slowly push an amp of sodium bicarb (one 50cc amp of bicarb is roughly equivalent to 100cc of 3% saline). Along with ABCs etc (will that fly on oral boards?).
If this isn’t urgent admit to L&D (MFM if you’ve got it), have medicine see them and fix their Na. Then same plan sans hyponatemic seizure.
NS is 154mEq of both Na+ and Cl-.
Interesting thank you. Would you then be concerned with myelinolysis?
My thinking was, you're using a tiny needle and not really removing fluid. This risk seemed small to negligible in my mind but I may be way off base.My concern would by herniation in the setting of elevated ICP

Gotcha, figured with the cerebral swelling there would be an auto correlation with increased icp, thanks for the correction
It appears I am the only one concerned with a spinal in patients with profound hyponatremia. Honestly I can say I have encountered many instances of having to consider spinal anesthesia in profoundly hyponatremic patients.
This is a spinal unless there’s no time for one? How in the world would you know that this is not acute on chronic hyponatremia? You’re right I’ve never seen brain herniation, coma, from profound hyponatremia.
if this is urgent and the patient has hyponatremia of unknown duration (at a minimum since her first set of pregnancy labs) then I wouldn’t be comfortable performing a spinal anesthetic on a patient on unknown brain swelling. I just wouldn’t. I haven’t run across this scenario since I’ve been an attending, and doubt I ran across this as a resident. You make it seem like you’ve seen this scenario daily and I should be confident that doing an intrathecal anesthetic is not a big deal.
“The most striking and severe symptoms of HNE are related to the compression of the brain parenchyma against the rigid skull. In severe cases, brain herniation and death often occurs preceded by seizures and coma. As discussed earlier, these symptoms often occur during acute and profound hyponatremia because the brain has no or little time to adjust to hypo- osmolality. “
“Parturients with intracranial lesions are often assumed to have increased intracranial pressure (ICP), and the risk of herniation is frequently cited as a contraindication to neuraxial anesthesia.11–18 To care for these parturients and ascertain which of them can safely undergo spinal or epidural analgesia or anesthesia;19–21 we must understand the factors that contribute to clinically significant brain tissue shifts (i.e., brain herniation), such as increased ICP, brain edema, or hydrocephalus. Anesthesiologists can then most effectively weigh the relative risks and benefits of neuraxial anesthesia for these patients and engage in productive multidisciplinary peripartum planning.”
“
Because epidural placement always entails the risk of a dural puncture even in the experienced hands,71 it is never a completely safe alternative if a spinal anesthetic is contraindicated. This is especially true because when inadvertent dural puncture does occur during epidural placement, it is with a much larger gauge needle. Conversely, even a small-gauge spinal needle causes a dural tear and potential CSF leak, so spinal anesthesia is not without risk when seeking to avoid significant loss of CSF.”
“In summary, there are no published randomized controlled trials comparing the safety of neuraxial versus general anesthesia in patients with intracranial lesions, nor are there likely to be any. As with all published case reports, there is an inherent bias in the cases that are chosen for reporting. Therefore, for each parturient with an intracranial lesion, there needs to be a collaborative team discussion, which includes anesthesia, obstetric, neurologic, and neonatology experts, and a rational exploration of the likelihood of increased ICP and the potential for related negative effects. To make recommendations on the proper anesthetic choice for any individual case, it is necessary to evaluate the relative contribution of each of the identified risks, in both severity and likelihood, and weigh them against the potential benefits.”
I’m not trying to convince anyone of anything. I asked what anesthetic people would choose. I next asked if there would be a concern about performing a spinal anesthetic in an unclear picture of profound hyponatremia in a setting of possible cerebral edema. I didn’t give much detail, out of any design as you claim other than to have an intellectual discussion. You seem preoccupied with my knowledge base, skill, and deriding my thoughtful questions. Asking questions and raising concerns about how I would perform an anesthetic in a novel scenario in a complex patient, yes is hand wringing, I would rather hand wring now, when all that is at stake for me is having some rando on the internet belittle me, than hand wring and potentially encounter a disastrous situation in real life. This should be a forum to explore complex or non complex issues free from harassment and degradation of others clinical competence. You seem to have a massive chip on your shoulder and don’t like anyone asking questions. I understand you know it all, this is all very gauche for you, but perhaps us common folk can ask questions without you haranguing us and calling us stupid.
Then do GA. Quit wringing your hands and clutching your pearls over it. As you presented the case is urgent. So get on with it. No one in that room is suffering (except maybe the patient's birth plan.....) if you do GA and know what you're doing.
I don't make it seem like this is a scenario we run into daily. We don't. There are lots of scenarios we don't see daily, monthly, or even yearly but that doesn't in itself make them complex and it doesn't force one to go down some super complex decision making pathway. I am presenting you with a normal, well reasoned way of thinking through this not terribly complex scenario from the viewpoint of an anesthesiologist.
I've told you why I'd do a spinal. I'd defend my answer on the oral exam if presented with that scenario. However, you can just as easily defend GA or doing the case with an epidural or a CSE. That's part of the beauty of anesthesia.
You've not convinced me away from my default anesthetic for CS. You've given no details on the clinical exam for this patient and you've also given no details on why this case is urgent. Those are extremely important details that are helpful in the development of a plan for this patient. My guess is that you've avoided further details by design. Regardless, I've given you my reasoning and my plan based on very limited information.
I am gonna channel @FFP and call a snowflake a snowflake.How about if nobody's rude to anybody? There's no need.
Case discussions tend to go better though if there are consistent details, or an upfront "hey this is all hypothetical" statement. This thread almost reads like an annoying "guess what I'm thinking" conversation with an attending.
I am gonna channel @FFP and call a snowflake a snowflake.
Because apparently you are being rude after admonishing rudeness.
Where did this person come from?
Haha
MeaCulpa said:Hi vac1476! I would love to hear more about ur experience at lecom. I'm a junior in high school
And my dad is a do from
Une. Thanks!
Please don’t tell me we are entertaining a child.They came from here:
Either Mea has a kid posting with their username or they're the snowflakiest of the snowflakes, or both.
Shout out to the author who i was in class with in med school!This paper explains why ICP doesn’t rise as expected in hypo-osmolar states.
Please don’t tell me we are entertaining a child.
Mods @Arch Guillotti, could you do something about this please? A child pretending to be someone they are not? Isn’t that some kind of TOS violation?
Well let's see, I am a hysterical worm, @pgg is rude and @Southpaw is petty, all of us getting vaccinated are a bunch of sheep and ......I’m annoying people who waste time of everyone involved. I will be blocking you thanks for the suggestion. Don’t speak for everyone else. Plenty of people have been able to answer questions in an appropriate manner, you hysterical worm.
you have done/considered many cases of spinal in profoundly hyponatremic patients?It appears I am the only one concerned with a spinal in patients with profound hyponatremia. Honestly I can say I have encountered many instances of having to consider spinal anesthesia in profoundly hyponatremic patients.
When it's an emergency and the pt. has to be put to sleep.What does no time for a spinal mean?
Hypothetically no.So prop sux tube don’t work in this hypothetical situation?
You're not telling us anything we don't already know. All of your quotes are pretty basic stuff for the anesthesiologist, and it's stuff you should already know as an attending. I don't know why you're posting it. What specifically about this patient, other than Na 115-120, should put the laryngoscope in my hand?