Can someone tell me why this is the case?
The way I am thinking is that in physiologic dead space, 100% oxygen goes to alveoli, but it is not perfusing. Like there is a barrier that prevents oxygen to cross alveoli and into the capillary.
So no matter how much oxygen we have in alveoli, it won't be able to cross to capillary? That was my logic. If someone can correct me, I would appreciate it.
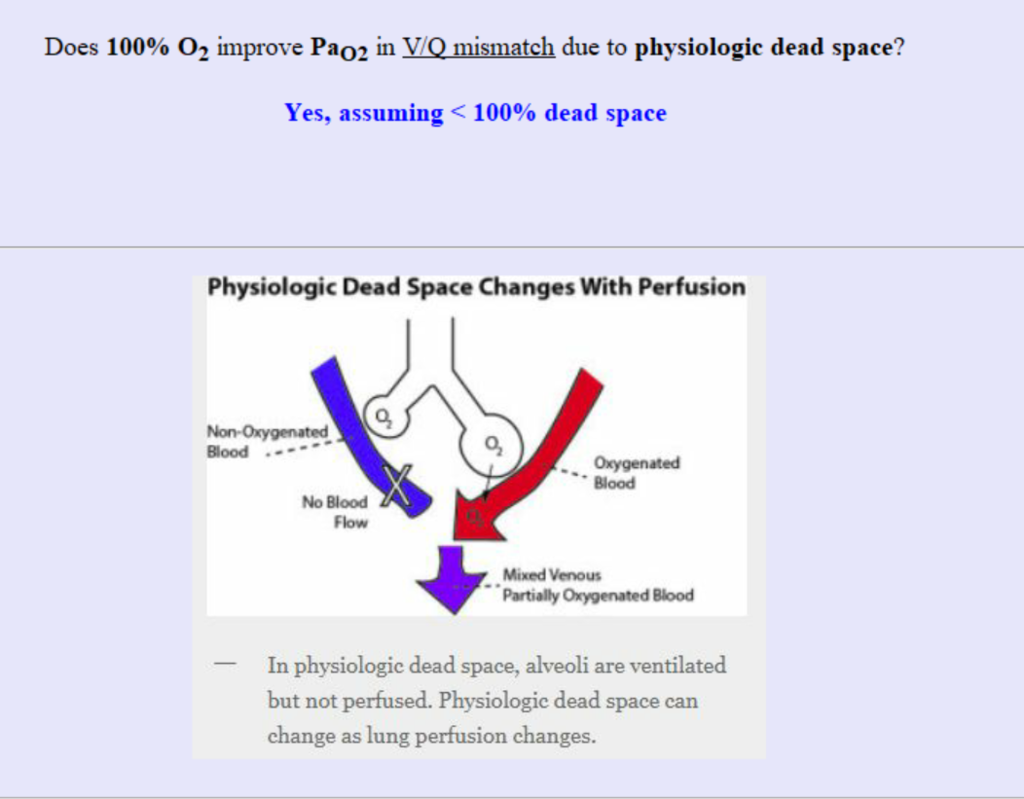
View attachment 225403
So, you have three different scenarios.
1. Shunt - this is a block of some of the alveoli that prevents gas diffusion into the capillary. If you give 100% O2, there will be no change in the PaO2 as some alveoli are not "working properly" to allow diffusion. The alveoli that are working properly are already working at their maximum capacity to make up for the others, so there is no additional gain in PaO2.
2. Physiologic dead space - this is where the alveoli are working properly, but there is a blood flow obstruction preventing perfusion of some of these alveoli (thus these vessels are not contributing to PaO2 at all). However, because the alveoli are working properly at their maximum capacity in other areas that are perfused,
you would not get hypoxemia with dead space alone. The main problem is increased PCO2 since the alveoli near the obstructed vessels cannot extract the CO2 from the obstructed vessels.
3. V/Q Mismatch
due to physiologic dead space - again, dead space in and of itself cannot cause hypoxemia. However, after some time passes, the obstruction of blood flow will be so great that it will actually divert the excess blood flow to the capillaries that are not obstructed. This leads to a V/Q of infinity in the obstructed areas (dead space) but a
decrease in V/Q in other areas due to excessive increase in flow (thus V/Q mismatch).
Your question relates to scenario 3. When you give 100% O2 to someone with V/Q mismatch due to physiologic dead space, the PaO2 improves. This is because the areas with the low V/Q due to excessive blood flow are now benefiting. Normally, blood is moving too fast to properly extract oxygen from the alveoli (normally inspired air has 21% O2). If you give 100% O2, you essentially have better odds of extracting more O2 (thus increasing PaO2). Again, the obstructed side is not perfusing and thus not even contributing to the PaO2.
Hope this long explanation helps!