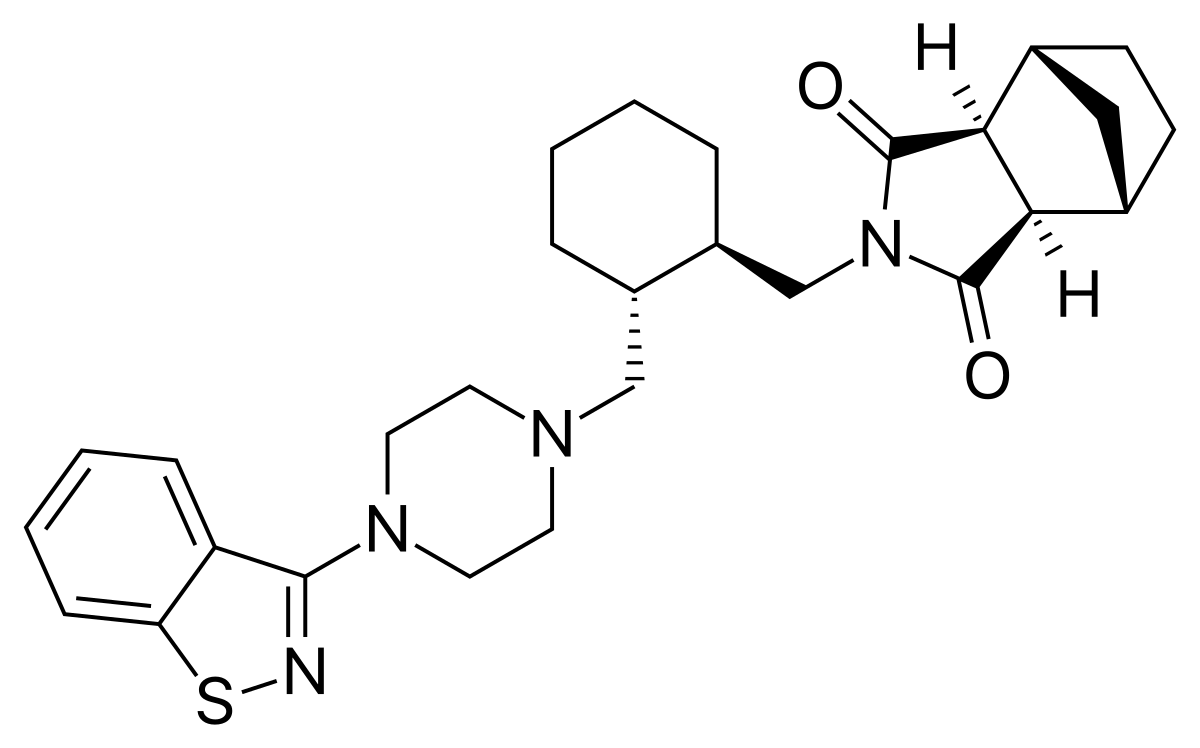
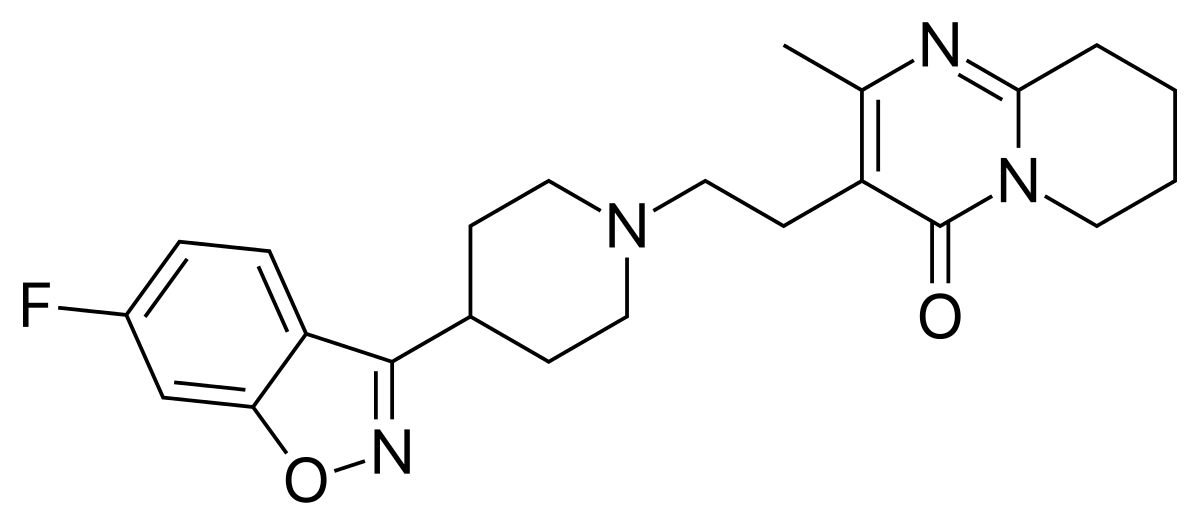
Look at these structures and tell me with a straight face that they're anywhere near "similar enough" that they're just one or two molecules off.
They do have similarities. I can say that with a straight face. I can say that as straight as I can say 1+1=2, but the problem is answering, "
that they're anywhere near "similar enough" that they're just one or two molecules off.
Cause this doesn't make sense unless you're just being way too easy.
A molecule by definition is a collection of bonded atoms, so I could literally just cleave off 2 collections of atoms (hence 2 molecules off) and the same -idone backbones would be there. I could still meet your challenge by erasing everything other than the idone backbone and that'd be 1-2 molecules.
I'm trying to be fair cause I figure maybe you didn't type what you meant-Yes Risperidone and Lurasidone do have similarities, and I never said those specific 2 are "one or two off." 1-2 molecules off, I'm not sure what you mean by that or why that's relevant because 1 molecule could be thousands of atoms or just 2 atoms bonded together. In terms of chemical metrics using "1-2 molecules off" has almost no relevance as far as I can see in terms of discussing pharmacology in the context above as far as I can tell. So I'm a bit confused with your sentence. If I did anything to create this confusion I apologize, but I'm not sure if I did.
Here's an example of just 1 molecule off.
"1995 biologists smashed records by cloning the DNA for the largest protein molecule known. The aptly named titin weighs in at a molecular weight of 3 million and consists of a continuous chain of 27,000 amino acids, making it 20 to 50 times larger than the average-size protein."
See what I mean? Your challenge that I say with a "straight face" that it's just 1-2 molecules off is as easy as me cutting a Gordian Knot with a knife. So I think you really didn't mean what you literally wrote.
A small change makes the most efficacious antipsychotic the least efficacious.
As I already stated above. I used the example of H20 vs H202, and Clozapine vs Quetiapine.
(Again Person X: Tell me with a straight face that 1+1=2, Person Y: Sure. 1+1=2).
Quetiapine and Clozapine have chemical similarities in structure, yet their differences make one the most efficicious antipsychotic, the other the least efficacious. I find it odd that you're using a point I already mentioned, acknowledged, and said in the context that this makes my argument one for weak consideration, but still of some consideration. (That's called nuance). Unless you're saying that cause you're supporting my argument? (which I don't get given the tone of the post).
But now getting to the other side of the sword, Quetiapine and Clozapine's similarities are indisputable and not on simpy a superficial level of just having the same suffix, but also chemical structure, similar receptor binding profiles, and several very similar side effects-weight gain, lipid increases, neutropenia, anticholinergic, etc. Clinically, the effects of both meds if given separately to two group of subjects, 20 each, could be difficult to distinguish among even experienced psychiatrists except for the efficacy of the antipsychotic benefit. (Very few side effects would distinguish them, one being hypersalivation). Among the several dozens of possible effects a med could have, one cannot deny that 2 meds, similar structures, simliar binding profiles, having amost the same effects on a person except for the 1 best intended effect (antipsychotic) still is a worthy argument.
The "idones" are incredibly dissimilar.
They can be, as they can also have similarites. Palliperidone as mentioned above, is almost identical to Risperidone. I can say that as straight as I can say 1+1=2.
Also, no idea why you're acting like it's the "apines" that cause agranulocytosis. It's literally every single antipsychotic that causes it.
Not all antipsychotics cause it in same degrees. You're arguing without acknowledging the known differences, of which still are poorly understood. This actually is something in our field rarely studied except for Clozapine, but of the data that exists, and just 1 study-THREE OF FOUR BIGGEST OFFENDERS ARE THE APINES.
Neutropenia and agranulocytosis (N&A) are relatively rare, but potentially fatal adverse drug reactions (ADR). This study presents cases of N&A related to one or more antipsychotic drugs (APDs) in psychiatric inpatients. Data on APD utilization and ...

www.ncbi.nlm.nih.gov
"A total of 124 cases of APD-induced N&A were documented, 48 of which fulfilled the criteria for agranulocytosis"
"Clozapine had the highest relative risk for inducing N&A and was imputed alone as a probable cause of N&A in 60 cases (1.57‰ of all patients exposed). Perazine showed the second highest relative risk with 8 cases and an incidence 0.52‰, followed by quetiapine (15 cases resp. 0.23‰ of all patients exposed) and olanzapine (7 cases; 0.13‰ of all patients exposed)."
Also, and the data is much older because typical antipsychotics aren't used as much, older data suggested phenothiazines tended to do it more vs the other typical nonphenothiazines. ("But they all cause neutropenia"-I never said they didn't). You're ignoring the nuance and using a black and white perspective, ignoring several dots that if connected together like the study above showing -apines may be, again MAY BE, ONE MORE TIME MAY BE (remember this is science, it's a stepwise progression to understanding) more of a problem with neutropenia vs the others. Remember what I wrote above? This type of stuff is worthy for the hypothetical stage of thought. SCIENCE INCLUDES HYPOTHESIS, NOT JUST CONCLUSIONS.
Mirtazapine has an association with neutropenia.
Neutropenia associated with mirtazapine use: is a drop in the neutrophil count in a symptomatic older adults a cause for concern?

pubmed.ncbi.nlm.nih.gov
Now one could say, "hey you're wrong Perazine causes neutropenia." I never said it didn't. One could say, "so you're saying Mirtazapnie is an antipsychotic?" I never said it was. One could say other psych meds cause neutropenia. I never said they didn't. One could say idones aren't identical-I never said they were identical. .......etc.
(I will say, however, that Mirtazapine is also having several similarities with apines. Which brings up to me a question-is there something going on with the benzene rings and formation of nitrenium ions? Nitrenium ions have benzene ring backbones as found in the apines, these ions are one of the proposed mechanisms cause oxidant damage to the bone marrow that causes neutropenia).
The -idones and the -apines aren't just suffixes. They correlate to backbone structures in the molecules. That's why quetiapine wasn't named BillyJoeBob. Again I said their similarities are for weak consideration, but (and I'm saying this again) sometimes that's all you got.