Hey! I am reading on some interesting presentations at ASTRO this year, mostly from Twitter.
I thought I'd make a thread to discuss on those.
Here's the first one:
Interesting findings, although not practice changing, in my humble opinion.
It will however make me feel more comfortable irradiating asymptomatic bone mets with more than just a gut feeling to back it up.
It will be interesting to see the breakdown of the SREs in the control arm, i.e. is there a true benefit for the patients or are we merely introducing RT earlier on but not changing any other endpoints (fractures, hospitalizations, surgeries).
I would not overemphasize the overall survival benefit. KPS was also significant in the MVA and there was an imbalance in the trial with the intervention arm having more patients in excellent KPS than the control arm, something which is not uncommon in Phase II trials.
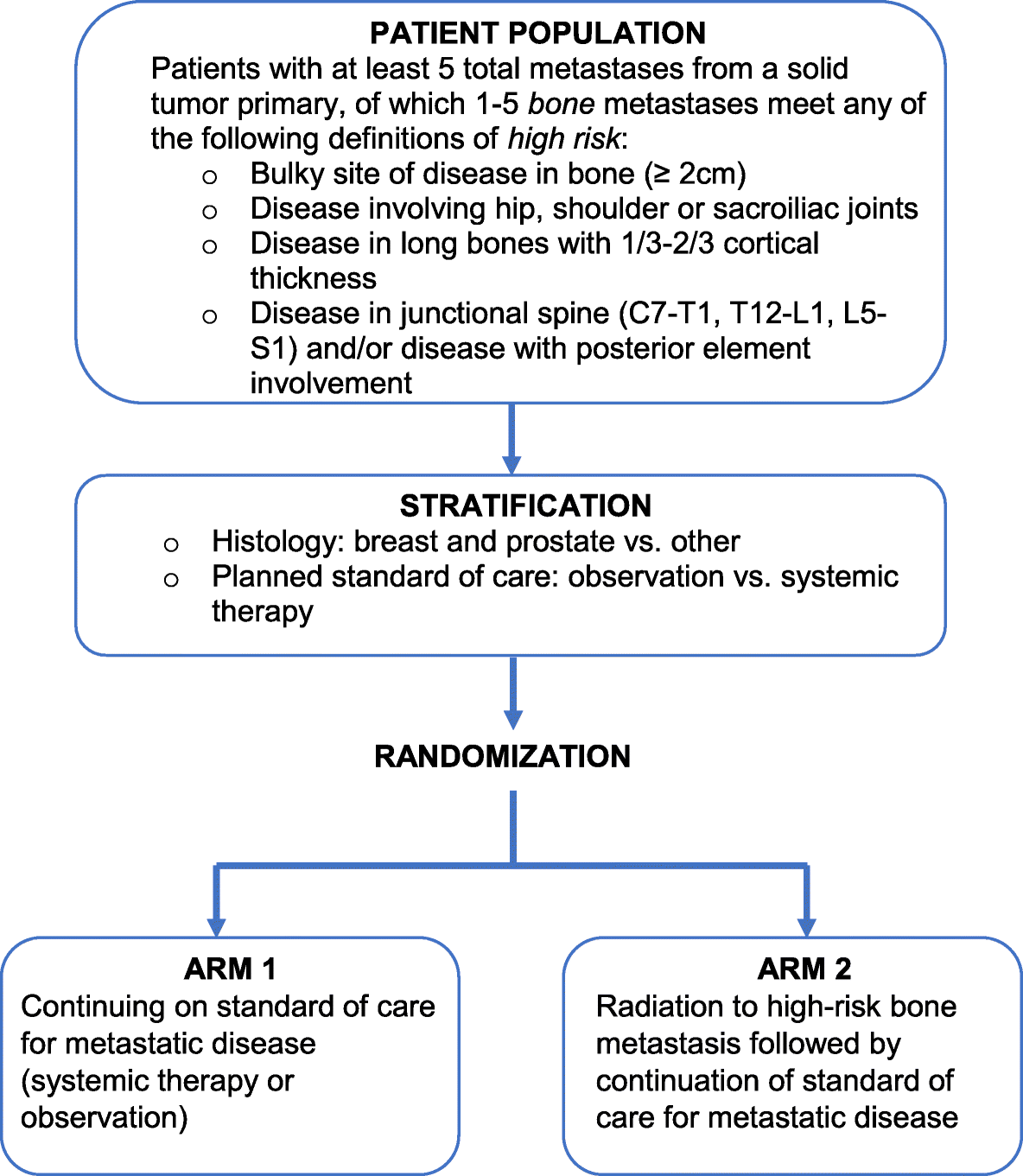
The protocol of the trial has been published before, for those of you that may have protocol-relevant questions:
Background In patients with metastatic cancer, the bone is the third-most common site of involvement. Radiation to painful bone metastases results in high rates of pain control and is an integral part of bone metastases management. Up to one-third of inpatient consults are requested for painful...

bmccancer.biomedcentral.com
Interesting point: They randomized 93 patients, although they had "planned" to randomize only 74 per protocol. The incidence of SREs in the trial appears to have been lower that what they had thought?
DISCUSS!