- Joined
- Jul 6, 2004
- Messages
- 1,977
- Reaction score
- 563
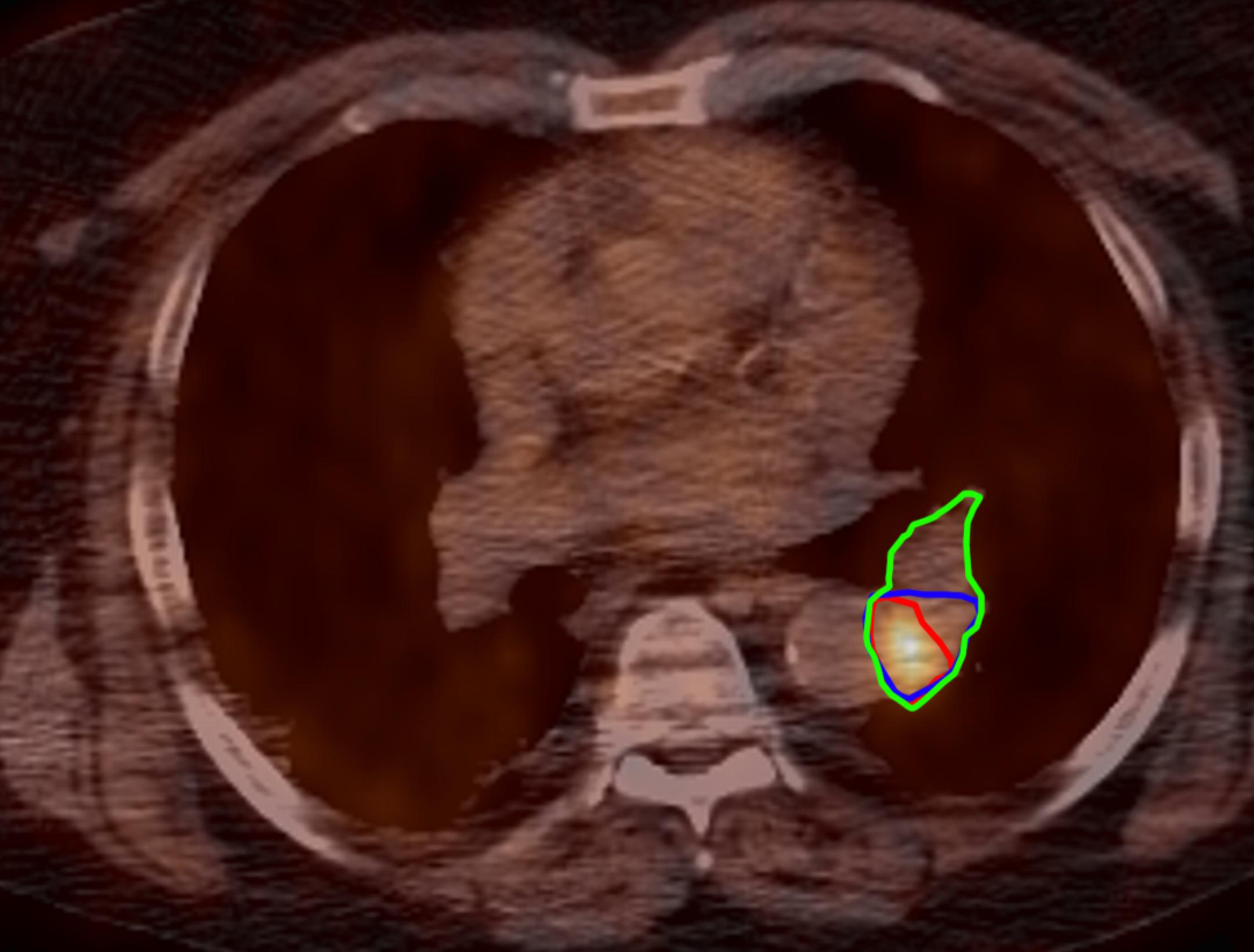
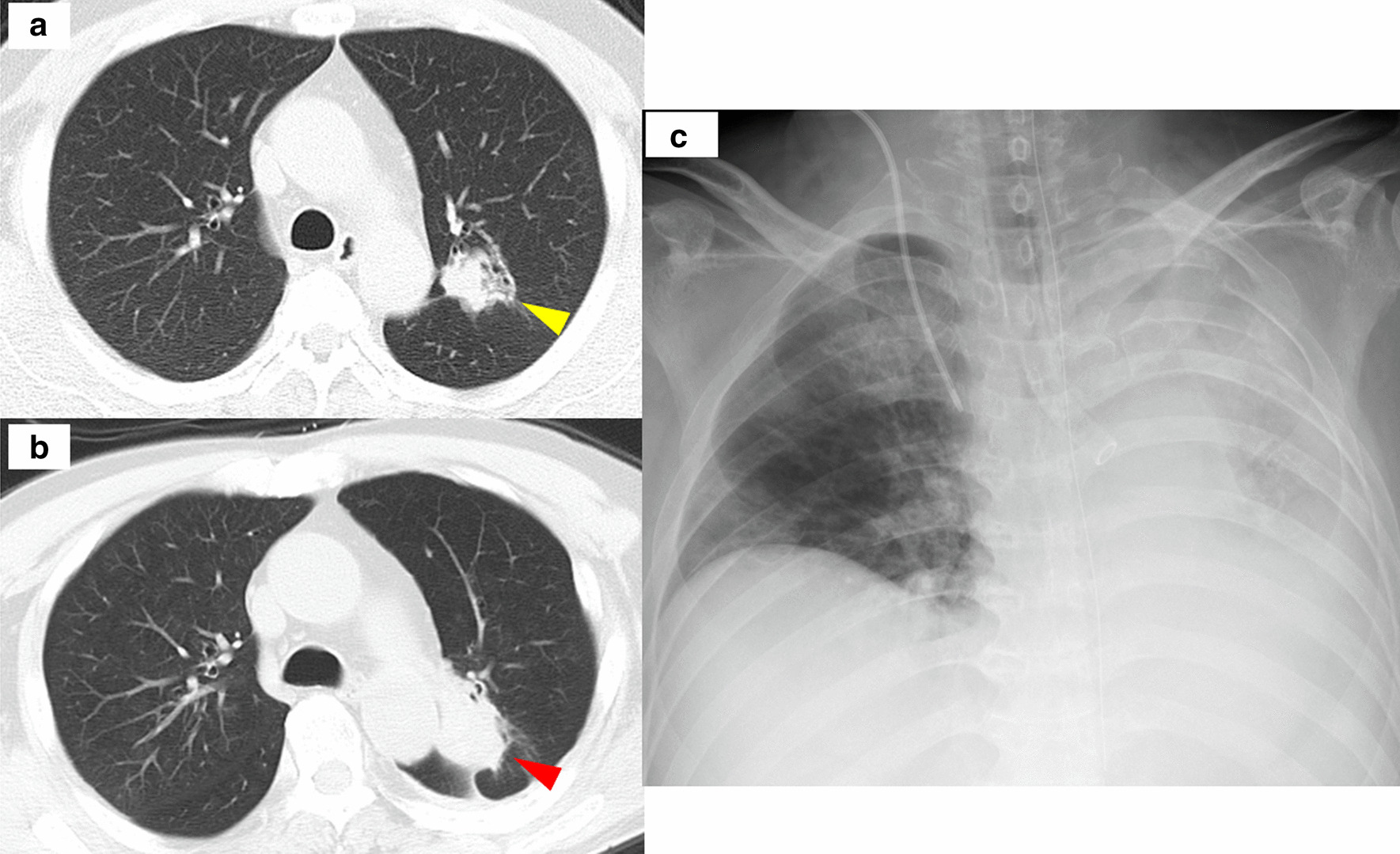
69 yo man with COPD and ILD with Wegeners Granulomatosis (GPA) on 2-3L O2 at rest and 3-4L on exertion gets rituxan infusions and on chronic steroids for the GPA had incidentally found 3.5 cm perihilar mass that is touching the aorta from about 2-5 o'clock. Biopsy positive for squamous cell carcinoma. Staged T4N0. Lung function is bad but sounds like he's been stable for over a year since starting rituxan in additionto the chronic steroids. Was just referred to us in RT and referred to med onc who he hasnt seen yet. Just curious what you guys think. I suspect we dont have much of a choice but worry about really worsening his situation, his lungs look downright terrible. Should i consider referring for proton? Thanks