- Joined
- Oct 10, 2011
- Messages
- 9,003
- Reaction score
- 11,508
- Points
- 8,831
- Attending Physician
Advertisement - Members don't see this ad
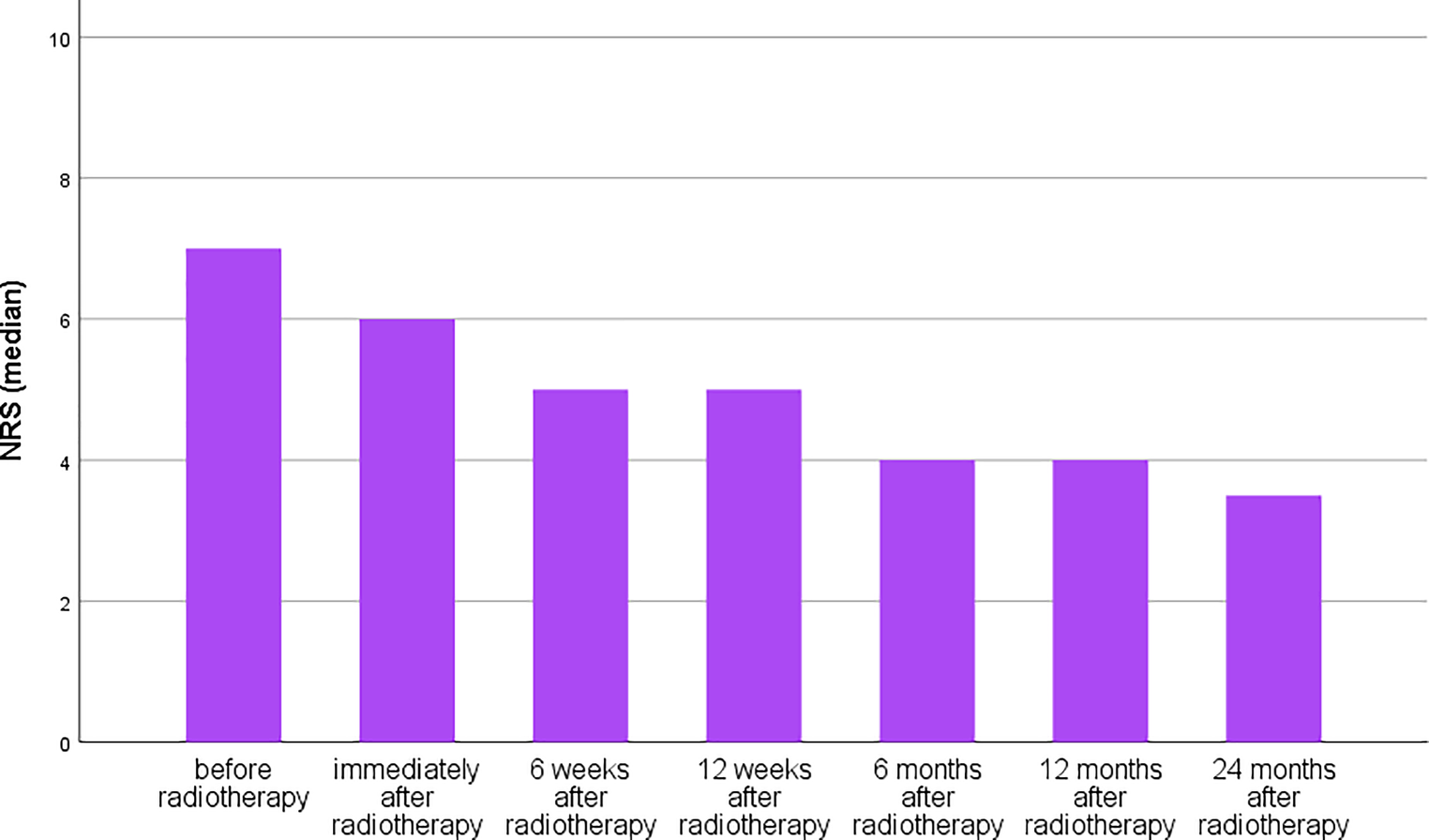
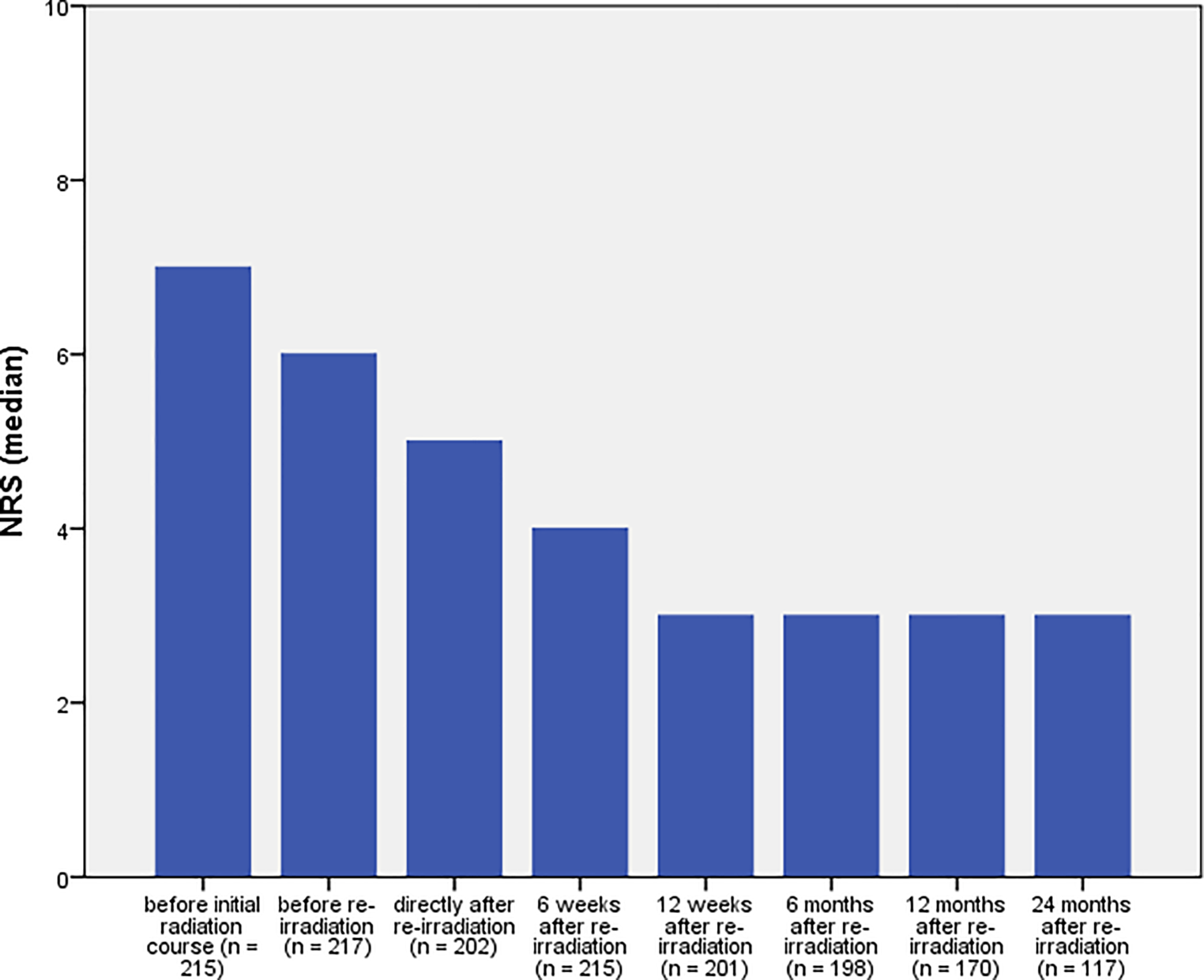
A "good sign" to predict response to treatment is an increase in pain immediately after the first fraction. This is something many you have seen when treating bone mets too, patients describe more pain after the first fraction which then fades off (some use steroids, there was even a randomized trial a while ago looking into that flare phenomenon).
"More pain" after the first fraction for arthritis treatment can be predictive for a durable response. However it's mostly seen in patients with an inflammatory component.
On a side note:
6 x 0.5 Gy has worked in a patient with atypical pain syndrome of the infraorbital nerve. Patient responded and remained pain-free for 2 years.
I was under the impression that 'pain flare' was a concern with high doses of radiation causing RT-induced inflammation compounding with a bone met. Things like 8Gy x 1, or SBRT dosing.
Are you expecting pain flare to be a thing at 0.5Gy?