You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Bone Scan vs PET Imaging Spin-Off
- Thread starter jondunn
- Start date
- Joined
- Sep 7, 2014
- Messages
- 3,616
- Reaction score
- 6,637
- Points
- 6,961
In a couple years when the psma pet era starts, the answer will be, no. Until then, the answer is, no.
In reality, it's nice to see et posting things his med mal insurer won't freak out about.
- Joined
- Sep 20, 2004
- Messages
- 12,511
- Reaction score
- 13,061
- Points
- 8,596
- Attending Physician
1) Some places don't have access to psma yet, only axumin 2) good luck getting it through evilcore on every patientIn a couple years when the psma pet era starts, the answer will be, no. Until then, the answer is, no.
In reality, it's nice to see et posting things his med mal insurer won't freak out about.
Evan clearly hasn't practiced in the real world yet, obviously many people will still be getting bone scans until it becomes more widely available and the insurers universally start covering it
- Joined
- Sep 7, 2014
- Messages
- 3,616
- Reaction score
- 6,637
- Points
- 6,961
Positive bone scans are useful for getting psma pets approved1) Some places don't have access to psma yet, only axumin 2) good luck getting it through evilcore on every patient
Evan clearly hasn't practiced in the real world yet, obviously many people will still be getting bone scans until it becomes more widely available and the insurers universally start covering it
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
so CVS is getting in the Rad Onc game? Former Rad Onc PD at UPENN, now swimming with the fishies over at CVS!
it's a wild world folks
View attachment 349313
Medical Director – Radiation Oncology at CVS Health
Medical Director – Radiation Oncology at CVS Health - Tarta.ai Job Search
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
Bone scans are also useful to check out false positive F18-PSMA findings in bones.Positive bone scans are useful for getting psma pets approved
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
What do you do with a bone+ PSMA followed by bone- bone scan. You'd have to biopsy?Bone scans are also useful to check out false positive F18-PSMA findings in bones.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
Honestly, since we have started getting those F18-PSMA scans for primary staging, I am tired of ordering second tests to verify PSMA findings.What do you do with a bone+ PSMA followed by bone- bone scan. You'd have to biopsy?
I've been ordering MRIs and bone scans, whenever I feel a certain PSMA finding may be fake.
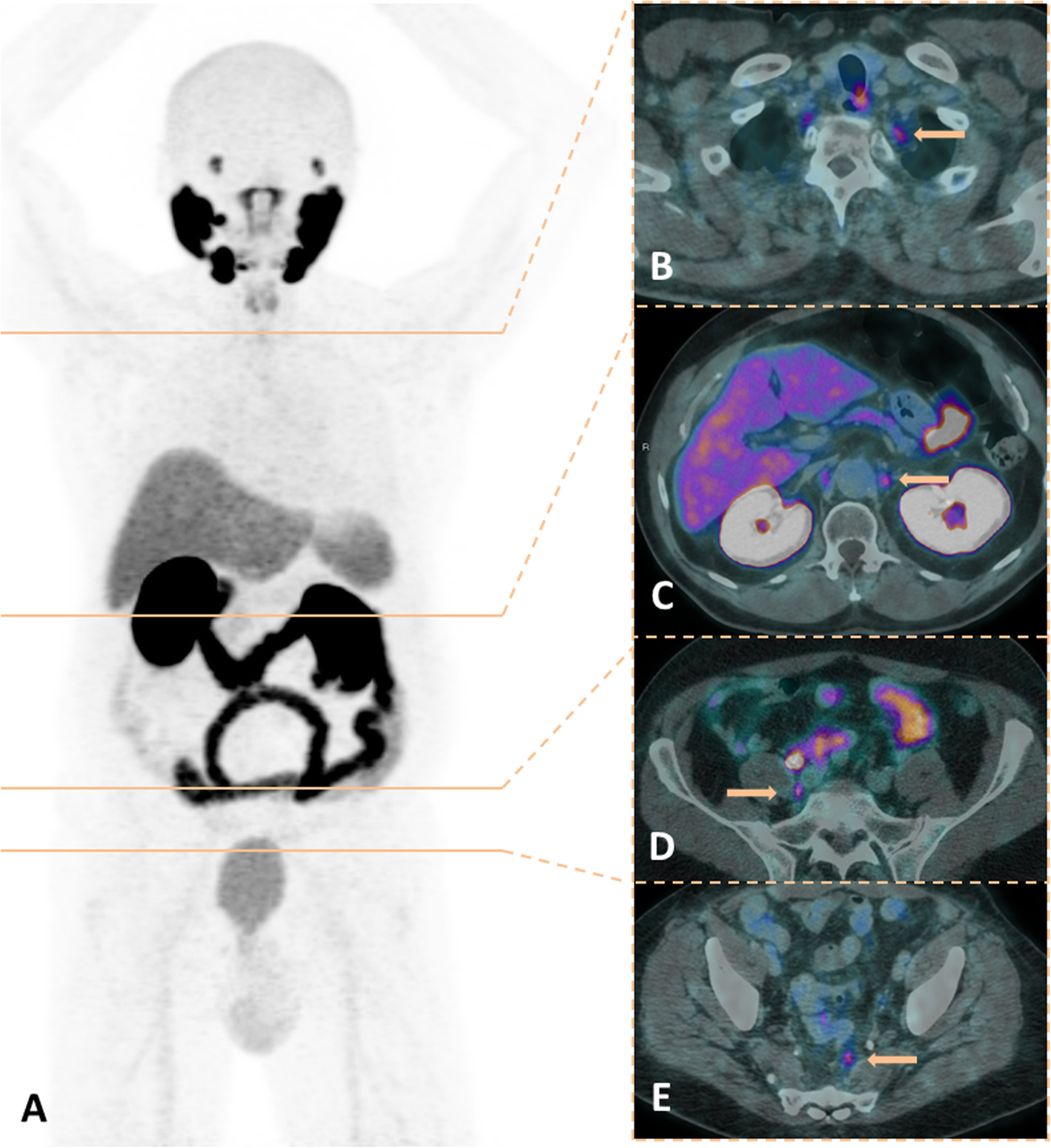
Latest example is this guy with an unfavorable, intermediate risk prostate cancer (T1c, GS4+3, PSA 14)
MRI came back completely negative. Absolutely nothing to be seen on that spot in the bone.
I am ignoring it, and treating prostate only with 4 months of ADT.
Last edited:
- Joined
- Feb 11, 2005
- Messages
- 605
- Reaction score
- 496
- Points
- 4,971
Palex- curious as to what that spot can be if not a metastasis ?
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
If we order a test and ignore the result of the test, why order a test in the first place 😉Honestly, since we have started getting those F18-PSMA scans for primary staging, I am tired of ordering second tests to verify PSMA findings.
I've been ordering MRIs and bone scans, whenever I feel a certain PSMA finding may be fake.
Latest example is this guy with an unfavorable, intermediate risk prostate cancer (T1c, GS4+3, PSA 14)
View attachment 349354
MRI came back completely negative. Absolutely nothing to be seen on that spot in the bone.
I am ignoring it, and treating prostate only with 4 months of ADT.
If PSMAs are positive only when another test makes them positive, PSMAs are a waste of money and needlessly anxiety inducing.
Advertisement - Members don't see this ad
- Joined
- Apr 11, 2009
- Messages
- 1,793
- Reaction score
- 1,875
- Points
- 6,466
- Attending Physician
I have seen a few weird spots in the posterior portions of the vertebral bodies near Batson’s plexus. It’s sort of like a different FDG; it’s very sensitive for prostate Mets but not necessarily specific.Palex- curious as to what that spot can be if not a metastasis ?
You also can get uptake in a lot of other stuff; psma is not specific. Hemangiomas, fibrous dysplasia, and many other things can have uptake but are not Mets.
I have a couple cases now where we are following the patient after local treatment to see if the vertebral uptake was a met or something spurious given the negative mri.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
That is an excellent question and I have no clue.Palex- curious as to what that spot can be if not a metastasis ?
F18-PSMA scans produce a large amount of false positives, especially in the ribs.
We biopsied one of these lesions once and it came back as a focal mastocytosis in the bone marrow.
That's potentially one differential diagnosis, apparently.
Hemangiomas are also another differential diagnosis, as Maxxor pointed out, which is why MRI can be helpful.
Last edited:
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
That's not exactly how it happened.If we order a test and ignore the result of the test, why order a test in the first place 😉
Someone else (urologist) ordered one test (PSMA-PET-CT) which came back positive, but I had doubts about this test result, so I ordered a second test (MRI) to verify the positive result of the first test (PSMA-PET-CT). That second test (MRI) came back negative. Bearing in mind, that the first test is known to produce false positives quite often (up to 50% according to some papers) and given the clinical history of the patient, I decided to trust the second test more than the first one. 🙂
Well, not necessarily. PSMA-PET-CTs can very well rule out metastatic disease that would have been visible with another diagnostic modality too.If PSMAs are positive only when another test makes them positive, PSMAs are a waste of money and needlessly anxiety inducing.
So, if your PSMA comes back negative, you can be pretty certain that whatever other test you would have ordered, would also have come back negative. The sensitivity of PSMA-PET-CT is superior to CT & bone scan combined. Some data point out that good whole-body MRIs are about as sensitive as PSMA-PET-CTs, but not everyone has access to those either and some patients cannot get them (claustrophobia, pacemaker. etc).
So, I am comfortable with ordering PSMA-PET-CTs for patients at high risk of metastatic disease (high-risk localized PCA or cN1) to rule out further metastasis that would have altered my therapeutic plan. I know however, that I may have to carry out further tests to rule out the false positive ones.
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
I don’t PSMA yet but you guys are confusing me. If you order a PSMA on a patient and you already expect they don’t have mets and the PSMA is negative, you proceed merrily along and everyone is reassured. If the PSMA is positive and you say well PSMAs give false positives and you do nothing, or get a different staging scan such as MRI that confirms your view that PSMA is often false positive… I don’t think at least statistically speaking the PSMA was wise to obtain in the first place.That is an excellent question and I have no clue.
F18-PSMA scans produce a large amount of false positives, especially in the ribs.
We biopsied one of these lesions once and it came back as a focal mastocytosis in the bone marrow.
That's potentially one differential diagnosis, apparently.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
Well, there is also Option 3: The PSMA comes back positive and you look very closely with an MRI (for instance) using all kinds of fancy things like DWI and confirm the diagnosis of a metastasis. Or you even order a biopsy and that comes back positive too.I don’t PSMA yet but you guys are confusing me. If you order a PSMA on a patient and you already expect they don’t have mets and the PSMA is negative, you proceed merrily along and everyone is reassured. If the PSMA is positive and you say well PSMAs give false positives and you do nothing, or get a different staging scan such as MRI that confirms your view that PSMA is often false positive… I don’t think at least statistically speaking the PSMA was wise to obtain in the first place.
Sometimes it's not just one lesion that will pop up in a PSMA-scan and prompt you to undertake action, often it's several lesions. So one odd false positive is common, but multiple false positives become less likely.
If you for instance have a patient with a high risk localized PCA and your conventional imaging shows nothing suspicious, but then you carry out a PSMA scan and it produces bilateral PSMA-positive lymph nodes in the pelvis and 1-2 nodes in the low retroperitoneal area (NOT enlarged nodes, just the common 5 mm familiar nodes we all see sometimes on CT-scans in the pelvis/retroperitoneum) and 2 lesions in the bony pelvis... well... that's probably a metastatic patient.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
My colleague gave a great journal club on this subject, here are 2 nice papers on this:

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
I am sorry for derailing this thread...

Focal unspecific bone uptake on [18F]-PSMA-1007 PET: a multicenter retrospective evaluation of the distribution, frequency, and quantitative parameters of a potential pitfall in prostate cancer imaging - PubMed
UBUs occur in two-thirds of patients imaged with [<sup>18</sup>F]-PSMA-1007 PET/CT and are significantly more frequent on digital PET scanners than analog scanners. UBUs should be interpreted carefully to avoid over-staging.

Matched-Pair Comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT: Frequency of Pitfalls and Detection Efficacy in Biochemical Recurrence After Radical Prostatectomy - PubMed
<span><sup>18</sup>F-labeled prostate-specific membrane antigen (PSMA)-ligand PET has several principal advantages over <sup>68</sup>Ga-PSMA-11. The purpose of this retrospective study was to evaluate the frequency of non-tumor-related uptake and the detection efficacy comparing...
I am sorry for derailing this thread...
- Joined
- Oct 10, 2011
- Messages
- 9,000
- Reaction score
- 11,503
- Points
- 8,831
- Attending Physician
My colleague gave a great journal club on this subject, here are 2 nice papers on this:

Focal unspecific bone uptake on [18F]-PSMA-1007 PET: a multicenter retrospective evaluation of the distribution, frequency, and quantitative parameters of a potential pitfall in prostate cancer imaging - PubMed
UBUs occur in two-thirds of patients imaged with [<sup>18</sup>F]-PSMA-1007 PET/CT and are significantly more frequent on digital PET scanners than analog scanners. UBUs should be interpreted carefully to avoid over-staging.pubmed.ncbi.nlm.nih.gov

Matched-Pair Comparison of 68Ga-PSMA-11 PET/CT and 18F-PSMA-1007 PET/CT: Frequency of Pitfalls and Detection Efficacy in Biochemical Recurrence After Radical Prostatectomy - PubMed
<span><sup>18</sup>F-labeled prostate-specific membrane antigen (PSMA)-ligand PET has several principal advantages over <sup>68</sup>Ga-PSMA-11. The purpose of this retrospective study was to evaluate the frequency of non-tumor-related uptake and the detection efficacy comparing...pubmed.ncbi.nlm.nih.gov
I am sorry for derailing this thread...
I'm at least learning something which I can't say the same for most of the other posts from RO twitter thread.
Time to move it to it's own thread!
- Joined
- Oct 10, 2011
- Messages
- 9,000
- Reaction score
- 11,503
- Points
- 8,831
- Attending Physician
I don’t PSMA yet but you guys are confusing me. If you order a PSMA on a patient and you already expect they don’t have mets and the PSMA is negative, you proceed merrily along and everyone is reassured. If the PSMA is positive and you say well PSMAs give false positives and you do nothing, or get a different staging scan such as MRI that confirms your view that PSMA is often false positive… I don’t think at least statistically speaking the PSMA was wise to obtain in the first place.
I mean... PSMA has relatively good specificity, but not greatest sensitivity. PSMA focally positive requires a kind of focal confirmation exam, which isn't practical to do for everybody (because unless you whole body MRI you wouldn't know where to look). The atlernative would be to proceed with a bone biopsy of that area, but if there's no CT correlate that's going to be tough as well.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
Actually, I find the sensitivity very good, superior to other modalities. It's the specificity where we have issues, mainly in the bones and especially with F18. Specificity for lymph nodes is very good, superior to CT/MRI (as long as not mistaken for ganglia).I mean... PSMA has relatively good specificity, but not greatest sensitivity. PSMA focally positive requires a kind of focal confirmation exam, which isn't practical to do for everybody (because unless you whole body MRI you wouldn't know where to look). The atlernative would be to proceed with a bone biopsy of that area, but if there's no CT correlate that's going to be tough as well.
- Joined
- Sep 7, 2014
- Messages
- 3,616
- Reaction score
- 6,637
- Points
- 6,961
God forbid we talk about doing two PSMA PETs, but in someone getting ADT, would repeating the PET after the PSA goes to zero be worthwhile in patients with equivocal results?
Advertisement - Members don't see this ad
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
Yeah to be clear. And there are exceptions to every rule, but… sensitivity implies believable negatives. Specificity implies believable positives. The specificity has a hill to climb in most cases of diagnostic tests because the pretest probabilities can be very low. Granted a positive can move that probability from say less than 1% to 50%, but would still bank on that 50%?Actually, I find the sensitivity very good, superior to other modalities. It's the specificity where we have issues, mainly in the bones and especially with F18. Specificity for lymph nodes is very good, superior to CT/MRI (as long as not mistaken for ganglia).
A more interesting question, in the vein of every action has an equal and opposite reaction, can a positive PSMA in 2022 move a patient that would have been metastasis negative in 2015 into a treatment track that may not be as survival prolonging (or as good QOL). I am sure we helped (in terms of survival, and minimizing global toxicity) many conventional imaging negative but actually metastatic patients in the past with good old localized prostate RT.
Last edited:
- Joined
- Apr 11, 2009
- Messages
- 1,793
- Reaction score
- 1,875
- Points
- 6,466
- Attending Physician
I have to agree with Palex here. On the spectrum of sensitive vs specific, it’s much more on the sensitive side. PSMA itself is a misnomer. It’s not specific and is expressed in lots of other tissues.Actually, I find the sensitivity very good, superior to other modalities. It's the specificity where we have issues, mainly in the bones and especially with F18. Specificity for lymph nodes is very good, superior to CT/MRI (as long as not mistaken for ganglia).
Bone scans will continue to be done for breast but I could envision a future where they stop being done for prostate. If only people would stop ordering them for RCC and TCC…
Nonprostatic diseases on PSMA PET imaging: a spectrum of benign and malignant findings - Cancer Imaging
PSMA PET imaging was originally used to assess biochemical recurrence of prostate cancer (PCa), but its clinical use was promptly extended to detection, staging and therapy response assessment. The expanding use of PSMA PET worldwide has also revealed PSMA ligand uptake in diverse nonprostatic...
- Joined
- Oct 10, 2011
- Messages
- 9,000
- Reaction score
- 11,503
- Points
- 8,831
- Attending Physician
Actually, I find the sensitivity very good, superior to other modalities. It's the specificity where we have issues, mainly in the bones and especially with F18. Specificity for lymph nodes is very good, superior to CT/MRI (as long as not mistaken for ganglia).
Think I messed up my definitions of sensitivity/specificity. Haven't had to think about that in a while. Reverse em in post above.
- Joined
- May 7, 2014
- Messages
- 1,780
- Reaction score
- 3,834
- Points
- 5,966
- Attending Physician
Easy mnemonicThink I messed up my definitions of sensitivity/specificity. Haven't had to think about that in a while. Reverse em in post above.
SpIN- Specificity rules something in
SnOUT- Sensitivity rules something out.
In general PSMA is highly specific (95%; especially LN) but moderately sensitive. 40% of PSMA negative high-risk prostate cancer patients are found to have node-positive disease at lymphadenectomy
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
FWIW I just tried to solve a system of equations where, assume 25% of high risk patients will be node+ at surgery:Easy mnemonic
SpIN- Specificity rules something in
SnOUT- Sensitivity rules something out.
In general PSMA is highly specific (95%; especially LN) but moderately sensitive. 40% of PSMA negative high-risk prostate cancer patients are found to have node-positive disease at lymphadenectomy
| 25% nodal risk at surgery (+ nodes) | 75% are node negative at surgery | |
| PSMA + | A | B |
| PSMA - | C | D |
Where C/(D+C)=0.4 (false omission rate), D/(B+D)=0.95 (specificity)... and the equation yields negative numbers for A. Which is to say I do not think C can be this
EDIT
If re-ran assuming the pre-surgery N+ incidence can be as high as 60%, then:
| 60% nodal risk at surgery (+ nodes) | 40% are node negative at surgery | |
| PSMA + | A = 347 | B = 20 |
| PSMA - | C = 253 | D = 380 |
satisfies a 95% specificity (B/[B+D]) and ~40% false omission rate (C/[C+D]) meaning that PSMA would have ~57% sensitivity in this totally made up hypothetical using your assumptions, and my N+ incidence assumption(s).
The sensitivity of PSMA (for nodes) will go up with the likelihood that the patient is N+. The test becomes worthless (ie "A" goes negative) somewhere less than between 35% and 40% pretest N+ probability. That is to say, if nomograms don't suggest a >40% N+ probability, a negative PSMA is very worthless.
Last edited:
- Joined
- May 7, 2014
- Messages
- 1,780
- Reaction score
- 3,834
- Points
- 5,966
- Attending Physician
Here is the paper I used for the Sp and Sn quoted.

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
Cohort A is germane to staging high risk patients
It is important to remember that Sp and SN are inherent to the test. Fiddling with the baseline rate can change PPV, NPV and "accuracy" but the Sn and SP are inherent and don't change.
Most papers on diagnosis are garbage; they should try to follow the STARD guidelines
What Wallnerus is getting at was studied in a paper recently released online. The setting is different however (recurrence after definitive therapy) but the motivating principle is the same-

 pubmed.ncbi.nlm.nih.gov
pubmed.ncbi.nlm.nih.gov
TBL
The original nomogram exhibited excellent characteristics on external validation. The incidence of a false negative scan can be reduced if PSMA-PET is performed when the predicted probability is ≥20%.

A Phase 2/3 Prospective Multicenter Study of the Diagnostic Accuracy of Prostate Specific Membrane Antigen PET/CT with 18F-DCFPyL in Prostate Cancer Patients (OSPREY) - PubMed
The primary end point for specificity was met while the primary end point for sensitivity was not. The high positive predictive value observed in both cohorts indicates that <sup>18</sup>F-DCFPyL-positive lesions are likely to represent disease, supporting the potential utility of...
Cohort A is germane to staging high risk patients
It is important to remember that Sp and SN are inherent to the test. Fiddling with the baseline rate can change PPV, NPV and "accuracy" but the Sn and SP are inherent and don't change.
Most papers on diagnosis are garbage; they should try to follow the STARD guidelines
What Wallnerus is getting at was studied in a paper recently released online. The setting is different however (recurrence after definitive therapy) but the motivating principle is the same-

Multicenter External Validation of a Nomogram for Predicting Positive Prostate-specific Membrane Antigen/Positron Emission Tomography Scan in Patients with Prostate Cancer Recurrence - PubMed
A nomogram has been developed to predict prostate-specific membrane antigen/positron emission tomography (PSMA-PET) results for recurrent prostate cancer (PCa). The nomogram represents an easy tool in the decision-making process of recurrent PCa.
TBL
The original nomogram exhibited excellent characteristics on external validation. The incidence of a false negative scan can be reduced if PSMA-PET is performed when the predicted probability is ≥20%.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
This is correct, in terms of sensitivity compared to pathology virtually every imaging will not be sensitive enough. We see that in every disease.Easy mnemonic
SpIN- Specificity rules something in
SnOUT- Sensitivity rules something out.
In general PSMA is highly specific (95%; especially LN) but moderately sensitive. 40% of PSMA negative high-risk prostate cancer patients are found to have node-positive disease at lymphadenectomy
But still, sensitivity of PSMA-PET-CT is higher than of CT (for instance) for detecting nodal metastasis prior to surgery.
The same also applies to CT to an ever higher degree, since sensitivity of CT is lower. Yet, we still perform staging CTs, even in unfavorable intermediate risk patients.That is to say, if nomograms don't suggest a >40% N+ probability, a negative PSMA is very worthless.
Sure, a CT is cheaper than a PET-CT. However, if you compare the sensitiviness of CT and PET-CT, you will probably find more lymph node metastases per dollar by ordering PET-CTs than by ordering CTs. One could run the math for that.
The proPSMA trial is a good trial comparing CT and PET-CT.
Sensitivity of conventional imaging was 38% and PSMA-PET-CT 85% for nodal and distant metastases, respectively.
Last edited:
- Joined
- May 7, 2014
- Messages
- 1,780
- Reaction score
- 3,834
- Points
- 5,966
- Attending Physician
Rather than looking at Sn and Sp we should really be using likelihood ratios to determine clinical utilityThis is correct, in terms of sensitivity compared to pathology virtually every imaging will not be sensitive enough. We see that in every disease.
But still, sensitivity of PSMA-PET-CT is higher than of CT (for instance) for detecting nodal metastasis prior to surgery.
EBM - Evaluating a Diagnostic Test Study
med.mercer.edu
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
Yes, sens and spec by themselves really don't help me clinically unless I know they're 99+% or something. Few tests reach that level for both sens and spec, one of the reasons you had to get two different tests to confirm HIV+ (the first very sensitive, the second specific) back in the day.It is important to remember that Sp and SN are inherent to the test...
TBL
The original nomogram exhibited excellent characteristics on external validation. The incidence of a false negative scan can be reduced if PSMA-PET is performed when the predicted probability is ≥20%.
Glad that math wound up making at least partial sense. Another TBL: tests with sensitivities in the lower range (ie 60-80%) e.g. need to be ran where the condition is pretty common or the false negative rate gets too high.
As an aside 'cause you might be a geek like me, using A, B, C, and D as variables as shown below:

And going off your numbers of B/(B+D)=0.95 (the specificity rate you cited) and C/(C+D)=0.4 (the false negative or omission rate you cited), I just plug this in Wolfram Alpha and played with the A+C number, which is the incidence of disease, in a 1000 patient population...

At a nodal disease incidence of A+C=388 (out of 1000 patients), or 38.8%, this is the lowest that nodal disease incidence can be for PSMA to be a useful test. At A+C=387 or less (38.7% incidence or less), A becomes negative (an irrational result obviously as there can be no less-than-zero patient numbers). And at 38.8% disease incidence, holding the false negative rate at C/(C+D)=0.4, the positive predictive value would only be:
A/(A+B) = 2/5 / (2/5+153/5) = 1.2%!!!!
An amazing result which means when the disease incidence gets too low in a non-sensitive test, a positive result gives you a 99% chance that the condition is not present!
Advertisement - Members don't see this ad
- Joined
- May 7, 2014
- Messages
- 1,780
- Reaction score
- 3,834
- Points
- 5,966
- Attending Physician
You are saying the quiet part out loud. The PSMA vendors can't keep up with demand and patients are clamoring for it. Arguably the value of the test is limited except in very high risk patients.
Popular example of how innumerate doctors are
Question-If a test to detect a disease whose prevalence is 1/1000 has a false positive rate of 5%, what is the chance that a person found to have a positive result actually has the disease, assuming you know nothing about the person's symptoms or signs?
In a paper published years ago with students, residents and attendings the most common answer (50% of participants) was 95% Which is very very wrong.
Answer- If only 1 in a 1,000 people have the disease, testing 1,000 people would produce about 50 false positives and 1 correct identification; 1 divided by 51 is 1.96 percent.
Of course prostate cancer patients have the disease but the same innumeracy is present in patients and doctors alike
Popular example of how innumerate doctors are
Question-If a test to detect a disease whose prevalence is 1/1000 has a false positive rate of 5%, what is the chance that a person found to have a positive result actually has the disease, assuming you know nothing about the person's symptoms or signs?
In a paper published years ago with students, residents and attendings the most common answer (50% of participants) was 95% Which is very very wrong.
Answer- If only 1 in a 1,000 people have the disease, testing 1,000 people would produce about 50 false positives and 1 correct identification; 1 divided by 51 is 1.96 percent.
Of course prostate cancer patients have the disease but the same innumeracy is present in patients and doctors alike
- Joined
- Oct 10, 2011
- Messages
- 9,000
- Reaction score
- 11,503
- Points
- 8,831
- Attending Physician
I mean... but people biopsy off the test before dooming someone to M1 right? I guess besides like boosting LNs or something, but for bone mets, folks are biopsying? I had a guy who I biopsied after PSMA PET showed a solitary 'met' in the rib. Negative. Treated definitively and doing fine now...
- Joined
- Sep 7, 2014
- Messages
- 3,616
- Reaction score
- 6,637
- Points
- 6,961
Sounds like another abscopal effect case report. Prove me wrong.I mean... but people biopsy off the test before dooming someone to M1 right? I guess besides like boosting LNs or something, but for bone mets, folks are biopsying? I had a guy who I biopsied after PSMA PET showed a solitary 'met' in the rib. Negative. Treated definitively and doing fine now...
- Joined
- Jan 10, 2010
- Messages
- 2,757
- Reaction score
- 3,873
- Points
- 6,641
- Attending Physician
There is too little data for PSMA to be considered standard of care in the staging setting for most patients. Given the low pre-test probability of positive nodes or mets in intermediate risk patients, even with a reasonably high specificity, the PPV is often less then 50%.
More importantly, however, is we lack data that tells us what to do with the PSMA scan result. Say my unfavorable intermediate risk patient gets one and there is a bone lesion. Say it's real on biopsy. Does that mean no surgery? Does STAMPEDE local therapy in oligometastatic setting (by conventional imaging) apply to M0 by conventional imaging but PSMA positive?
Realistically a chunk of the patients we operate on/radiate for localized disease are undetectably (by conventional imaging) metastatic. If we omit the local therapy based on the PSMA, are we helping them? I would argue no based on data that patients without prostate who progress to metastatic disease have a much more favorable prognosis (caveats about selecting for disease biology applies), as well as STAMPEDE Data (and accumulating data for prostatectomy in M! disease) suggesting treating primary is effective even in the metastatic setting. Should we SBRT PSMA positive micromets along with local therapy? Maybe, but there's no data to guide this.
Personally my main use of PSMA is in the XRT failure group to determine local vs. distant failure and whether to consider salvage therapy for isolated local recurrence or SBRT for oligometastatic failure. But even that is a limited data zone.
More importantly, however, is we lack data that tells us what to do with the PSMA scan result. Say my unfavorable intermediate risk patient gets one and there is a bone lesion. Say it's real on biopsy. Does that mean no surgery? Does STAMPEDE local therapy in oligometastatic setting (by conventional imaging) apply to M0 by conventional imaging but PSMA positive?
Realistically a chunk of the patients we operate on/radiate for localized disease are undetectably (by conventional imaging) metastatic. If we omit the local therapy based on the PSMA, are we helping them? I would argue no based on data that patients without prostate who progress to metastatic disease have a much more favorable prognosis (caveats about selecting for disease biology applies), as well as STAMPEDE Data (and accumulating data for prostatectomy in M! disease) suggesting treating primary is effective even in the metastatic setting. Should we SBRT PSMA positive micromets along with local therapy? Maybe, but there's no data to guide this.
Personally my main use of PSMA is in the XRT failure group to determine local vs. distant failure and whether to consider salvage therapy for isolated local recurrence or SBRT for oligometastatic failure. But even that is a limited data zone.
- Joined
- Oct 10, 2011
- Messages
- 9,000
- Reaction score
- 11,503
- Points
- 8,831
- Attending Physician
@DoctwoB Seriously?
Nobody should not be doing prostatectomies off protocol in patients with known M1 disease. How the patient was determined to be M1 (but if there's pathologic confirmation) is immaterial. To me PSMA (with biopsy confirmation of metastatic disease) takes definitive local therapy off the table. I favor prostate RT (include LNs if involved) to 55/20 to those with 'limited disease' unless truly oligometastatic and you're going to go for a mix of STAMPEDE and ORIOLE/STOMP.
When MRI brain was developed, people did not ask if we should still routinely offer surgery in someone with local therapy because "historically we did CTs of the brain and treated some fraction of those already metastatic". And I'm not talking about like the rare case. It is a better imaging that shows metastatic disease better than previous imaging. That is the same story with PSMA PET vs CT/Bone scan.
The fact that we feel that omitting a local therapy in M1 disease needs evidence RATHER than the opposite is a telling sign of the field of Urology (and in fairness, certain Rad Oncs who believe we need to re-run everything in the PSMA era).
Urology is the same specialty that showed no OS benefit in CARMENA with RP, but still does it now because "IT is so much better now, so we need to re-run the trial". Same specialty that poo-poos prostate RT as per STAMPEDE b/c what about Abiraterone?!?!. Urology, the ultimate gunners - we want to get ours, and if we can't get ours then we'll make damn sure you can't get yours either!
Nobody should not be doing prostatectomies off protocol in patients with known M1 disease. How the patient was determined to be M1 (but if there's pathologic confirmation) is immaterial. To me PSMA (with biopsy confirmation of metastatic disease) takes definitive local therapy off the table. I favor prostate RT (include LNs if involved) to 55/20 to those with 'limited disease' unless truly oligometastatic and you're going to go for a mix of STAMPEDE and ORIOLE/STOMP.
When MRI brain was developed, people did not ask if we should still routinely offer surgery in someone with local therapy because "historically we did CTs of the brain and treated some fraction of those already metastatic". And I'm not talking about like the rare case. It is a better imaging that shows metastatic disease better than previous imaging. That is the same story with PSMA PET vs CT/Bone scan.
The fact that we feel that omitting a local therapy in M1 disease needs evidence RATHER than the opposite is a telling sign of the field of Urology (and in fairness, certain Rad Oncs who believe we need to re-run everything in the PSMA era).
Urology is the same specialty that showed no OS benefit in CARMENA with RP, but still does it now because "IT is so much better now, so we need to re-run the trial". Same specialty that poo-poos prostate RT as per STAMPEDE b/c what about Abiraterone?!?!. Urology, the ultimate gunners - we want to get ours, and if we can't get ours then we'll make damn sure you can't get yours either!
- Joined
- Jan 10, 2010
- Messages
- 2,757
- Reaction score
- 3,873
- Points
- 6,641
- Attending Physician
@DoctwoB Seriously?
Nobody should not be doing prostatectomies off protocol in patients with known M1 disease. How the patient was determined to be M1 (but if there's pathologic confirmation) is immaterial. To me PSMA (with biopsy confirmation of metastatic disease) takes definitive local therapy off the table. I favor prostate RT (include LNs if involved) to 55/20 to those with 'limited disease' unless truly oligometastatic and you're going to go for a mix of STAMPEDE and ORIOLE/STOMP.
When MRI brain was developed, people did not ask if we should still routinely offer surgery in someone with local therapy because "historically we did CTs of the brain and treated some fraction of those already metastatic". And I'm not talking about like the rare case. It is a better imaging that shows metastatic disease better than previous imaging. That is the same story with PSMA PET vs CT/Bone scan.
The fact that we feel that omitting a local therapy in M1 disease needs evidence RATHER than the opposite is a telling sign of the field of Urology (and in fairness, certain Rad Oncs who believe we need to re-run everything in the PSMA era).
Urology is the same specialty that showed no OS benefit in CARMENA with RP, but still does it now because "IT is so much better now, so we need to re-run the trial". Same specialty that poo-poos prostate RT as per STAMPEDE b/c what about Abiraterone?!?!. Urology, the ultimate gunners - we want to get ours, and if we can't get ours then we'll make damn sure you can't get yours either!
Agree prostatectomy should be in trial for M1 disease (with exceptions. If I have a patient who is in urinary retention and has low volume M1 disease, it will be discussed)
But you are wrong to suggest that there is likely not a difference biologically between micro/macrometastatic disease. We simply don't have the data to know the natural history of micrometastatic lesions in terms of rapidity of progression, are they a seed for additional mets, will SBRTing them make a difference given they represent a miniscule burden of disease and so on. Thought experiment: moving forward, we will probably have cell-free DNA assays that can identify prostate cancer DNA. Maybe we end up with a trial that shows us who will benefit from local therapy depending on that there cfDNA shows. But in the meantime, would you change your standard of care because the assay exists? I would argue similar for PSMA-PET. While level 1 evidence for prostatectomy is accruing, the proponderance of data (retrospective data, chinese RCT, belgian prospective registry, etc) all show benefit of prostatectomy in M1 disease, and likely the same or more so in conventional M0 PSMA M1 disease.
(American Urological Association)
(AUA 2021 Annual Meeting)
Role of surgery in oligometastatic prostate cancer - PMC
Androgen deprivation therapy as single modality therapy was the standard management for oligometastatic prostate cancer (PCa). Current paradigm shifts toward a multimodality therapy approach, targeting all sites of disease, including treatment of ...
FWIW all my oligometastatic PC patients get radiated. And WRT the CARMENA trial, I could talk your ear off about potential issues with the trial (very low accrual rate (<1 patient per center per year), underrepresentation of good/intermediate prognosis patients, poor use of systemic therpay in nephrectomy patients likely due to patient selection to begin with etc.), but the change in systemic therapy is a very real issue. Also keep in mind that the trial wasn't CN vs. no CN, it was up front CN vs. up front systemic therapy often with delayed CN. Big RCT showed benefit of cytoreductive nephrectomy in the era of IFN and IL-2 immunotherapy. RCT showed no benefit in era of TKI primary therapy. Now we are in the PD/PD-L1 era as first line therapy. Is cytoreductive nephrectomy helpful with this immunotherapy as it was with IFN/IL-2? Who knows? What I do know is that its highly patient specific and your broad generalizations are both untrue and unhelpful. Young 50 year old with ongoing bleeding and anemia or other paraneoplastic syndromes with vast majority of disease burden in kidney? Take it out. Frail 90 year old with brain and liver mets? Start immunotherapy and refer to hospice. And there is a lot of ground in the middle where the right answer is less obvious, though the trend has been more towards systemic therapy with consolidative nephrectomy depending on response.
Edit: Also keep in minds that PSMA has a significant false positive rate, especially in the settings where the pre-test probability is relatively low. If there is no conventional imaging correlate, how do you biopsy? (note: you can't). So you're going to tell me that a 60 year old guy with 2 cores of GG3 disease, a PSA of 9, and a PSMA lesion that has a decent shot of being a false positive shouldn't get surgery or radiotherapy with curative intent? I call Shenanigans.
Last edited:
- Joined
- Jul 28, 2009
- Messages
- 335
- Reaction score
- 100
- Points
- 4,681
- Attending Physician
I think our nuclear med physicians have read the most in the country (part of the original PSMA PET trial) but now I worry we're overtreating...
The PSMA+ but MRI- bone lesion patients here are reviewed at tumor board and usually get oligomet directed therapy.
The PSMA+ but MRI- bone lesion patients here are reviewed at tumor board and usually get oligomet directed therapy.
- Joined
- Sep 13, 2021
- Messages
- 2,023
- Reaction score
- 2,265
- Points
- 4,221
- Attending Physician
I think our nuclear med physicians have read the most in the country (part of the original PSMA PET trial) but now I worry we're overtreating...
The PSMA+ but MRI- bone lesion patients here are reviewed at tumor board and usually get oligomet directed therapy.
yeah interesting, I have not heard about this before - ignoring the MRI and treating anyways?
- Joined
- May 7, 2014
- Messages
- 1,780
- Reaction score
- 3,834
- Points
- 5,966
- Attending Physician
Local control of non-cancer approaches 100%yeah interesting, I have not heard about this before - ignoring the MRI and treating anyways?
Advertisement - Members don't see this ad
- Joined
- Jan 10, 2010
- Messages
- 2,757
- Reaction score
- 3,873
- Points
- 6,641
- Attending Physician
Fair. Meant palliative. Can't go to hospice without trying a little keytruda first.'Start immunotherapy and refer to hospice.'
this statement doesn't quite make sense.
- Joined
- Dec 17, 2007
- Messages
- 3,813
- Reaction score
- 5,483
- Points
- 6,441
- Age
- 45
- Location
- Europe
- Attending Physician
But you are wrong to suggest that there is likely not a difference biologically between micro/macrometastatic disease.
- Joined
- Nov 2, 2019
- Messages
- 3,601
- Reaction score
- 14,885
- Points
- 6,041
- Attending Physician
If you have 100 swans, and 96 are white but 4 are black...You are saying the quiet part out loud. The PSMA vendors can't keep up with demand and patients are clamoring for it. Arguably the value of the test is limited except in very high risk patients.
Popular example of how innumerate doctors are
Question-If a test to detect a disease whose prevalence is 1/1000 has a false positive rate of 5%, what is the chance that a person found to have a positive result actually has the disease, assuming you know nothing about the person's symptoms or signs?
In a paper published years ago with students, residents and attendings the most common answer (50% of participants) was 95% Which is very very wrong.
Answer- If only 1 in a 1,000 people have the disease, testing 1,000 people would produce about 50 false positives and 1 correct identification; 1 divided by 51 is 1.96 percent.
Of course prostate cancer patients have the disease but the same innumeracy is present in patients and doctors alike
p<0.05, all swans are white.
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
Journal of Nuclear Medicine, Jan 2022
Appropriate Use Criteria for PSMA Imaging
(The very low sensitivity is still concerning to me: when a patient truly has a nodal met, PSMA will very likely be positive... and when PSMA is positive, it is pretty likely the patient will not actually have nodal mets.)
Appropriate Use Criteria for PSMA Imaging
(The very low sensitivity is still concerning to me: when a patient truly has a nodal met, PSMA will very likely be positive... and when PSMA is positive, it is pretty likely the patient will not actually have nodal mets.)
- Joined
- Jan 10, 2010
- Messages
- 2,757
- Reaction score
- 3,873
- Points
- 6,641
- Attending Physician
Journal of Nuclear Medicine, Jan 2022
Appropriate Use Criteria for PSMA Imaging
(The very low sensitivity is still concerning to me: when a patient truly has a nodal met, PSMA will very likely be positive... and when PSMA is positive, it is pretty likely the patient will not actually have nodal mets.)
Actually the opposite. Low sensitivity means if patient has a nodal met good chance the PSMA is negative ( roughly 50/50).
High specificity sounds like if it is positive, should be a true positive but that is counteracted by low pre test probability of nodal Mets in most setting which means the positive predictive value is much lower then ideal.
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
I botched it.Actually the opposite. Low sensitivity means if patient has a nodal met good chance the PSMA is negative ( roughly 50/50).
“The very low sensitivity is still concerning to me: when a patient truly has no nodal met, PSMA will very likely be negative...but when PSMA is positive, it is pretty likely the patient will truly have no nodal met.”
- Joined
- Sep 7, 2014
- Messages
- 3,616
- Reaction score
- 6,637
- Points
- 6,961
This is still wrong isn't it? If psma positive, it's likely true, is psma negative, decent Chance it's a false negative.I botched it.
“The very low sensitivity is still concerning to me: when a patient truly has no nodal met, PSMA will very likely be negative...but when PSMA is positive, it is pretty likely the patient will truly have no nodal met.”
Edit. Yeah. As below, I thought about it more. There's a lot of ways to say the same thing, but its hard to think about how tests work from the cancer's point of view
Last edited:
- Joined
- Apr 3, 2019
- Messages
- 5,120
- Reaction score
- 11,694
- Points
- 5,601
- Attending Physician
This is still wrong isn't it! If psma positive, it's likely true, is psma negative, decent Chance it's a false negative.

“The very low sensitivity is still concerning to me: when a patient truly has no nodal met, PSMA will very likely be negative...but when PSMA is positive, it is pretty likely the patient will truly have no nodal met.”
It depends on the incidence. If you do the test and the incidence is too low (at sens=40%, spec=98%), this can be true. The incidence is the kicker. It can be the case that a positive PSMA in a node predicts very accurately for no nodal met. (EDIT: and this is sort of trickery on my part below; the pre-test N+ probability was ~1%, the post-test, 16.67%...)


Last edited:
- Joined
- Jan 10, 2010
- Messages
- 2,757
- Reaction score
- 3,873
- Points
- 6,641
- Attending Physician
Playing with MSKCC Nomograms, the PPV will usually be quite low due to low pre test probability of nodes.
It takes a patient with a PSA of 25, GG5 disease in 10/12 cores, and ct3b disease to get a 75% change of LN involvement and thus a high PPV.
Take a more typical patient, GG3 disease in 4 cores, PSA 10, cT2a. That’s a 15% incidence and thus a quite low PPV.
It takes a patient with a PSA of 25, GG5 disease in 10/12 cores, and ct3b disease to get a 75% change of LN involvement and thus a high PPV.
Take a more typical patient, GG3 disease in 4 cores, PSA 10, cT2a. That’s a 15% incidence and thus a quite low PPV.
- Joined
- Jun 18, 2015
- Messages
- 580
- Reaction score
- 680
- Points
- 5,096
- Resident [Any Field]
Also notice in the OSPREY cohort A, PSMA PET for pelvic nodes >5mm had a higher sensitivity (60%), so NPV was boosted about 10% (absolute).
“The very low sensitivity is still concerning to me: when a patient truly has no nodal met, PSMA will very likely be negative...but when PSMA is positive, it is pretty likely the patient will truly have no nodal met.”
It depends on the incidence. If you do the test and the incidence is too low (at sens=40%, spec=98%), this can be true. The incidence is the kicker. It can be the case that a positive PSMA in a node predicts very accurately for no nodal met. (EDIT: and this is sort of trickery on my part below; the pre-test N+ probability was ~1%, the post-test, 16.67%...)


Advertisement - Members don't see this ad
Similar threads
- Replies
- 7
- Views
- 2K
