- Joined
- Sep 19, 2018
- Messages
- 771
- Reaction score
- 564
Dear SDN Anesthesiologists
I hope you are doing well, bringing up a case for discussion.
Yesterday we had an interesting case for C/S - elective, she was prepared, fasting time roughly over 8 hours, patient is young, and once she laid supine, her pulse rate was exceeding 150 bpm, and sometime reached 170 bpm. Very vague, isn't it? Aside from being covid positive! BP 130/80 like normal!
Well, we were skeptical between to proceed with neuraxial vs GA, we decided to do ECG, appears sinus tachycardia only.
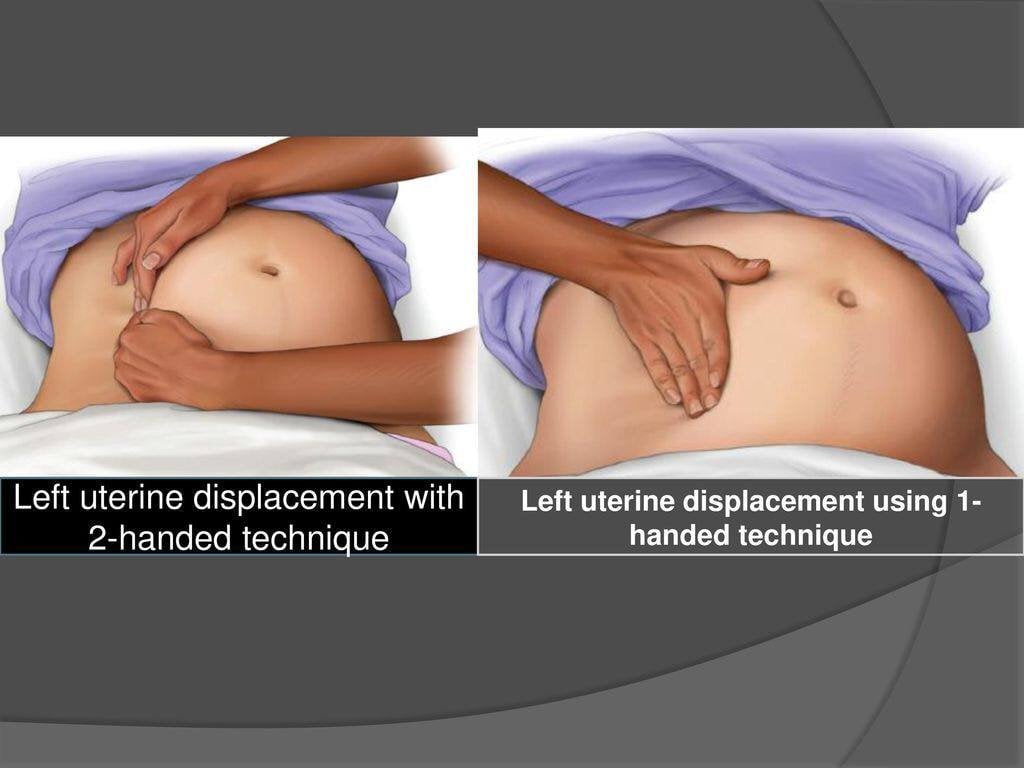
Two days ago, we were having a discussion about aortocaval compression, and one of the methods especially used for CPR in pregnants, are to do either one hand or two hand left side tilt of abdomen, it helps in CPR. Actually, I requested from our primary PGY1 residents to aid the discussion, and interestingly one of the residents shows us a picture of the procedure, which is very interesting. (one hand vs two hands)
Back to the patient, while she was supine, I tried to do two hands pressure towards the left side, and what was amazingly happened, is that her pulse rate dropped to 135 bpm!
I freed my hand, the Tachycardia increased between 150 to 160 bpm.
We weren't sure, why? Our Attending was at the bedside instructing us, and then we put (pint of fluid - no wedge pillow available) underneath the right iliac crest to create left tilting, but wasn't that much successful to reduce the heart rate even with plus bed tilting, unless I put my both hands again, the pulse dramatically dropped to 130s bpm. Then we assumed it is an aortocaval compression, but why normotensive? It should've be hypotension, sweating,,, etc isn't it? Patient wasn't even anxious.
We ask the patient to sit, like we are trying to do spinal, her pulse rate dropped to 130s, once she was back supine, it increased very fast to 165 bpm!
I kept my hands on again and dropped to 130s not even 140s, then we decided GA, and another PGY1 started her induction smoothly, and with scoline - RSI, once scoline in, I felt my push was much better and stronger to get PR of 120 bpm, and she tubed the patient with ease!
The OBGYNs residents c/s her fast, reached the baby, but it was obstructed too, they got the help of their Senior, and I removed the pint of normal saline from underneath the patient, and once the baby out crying to life, we got a PR fixed on 135 bpm, and the patient didn't go hypotensive at all or hypoxic, except lax uterus and we managed it by decreasing the isoflurane + giving oxytocine, and the tachycardia kept interestingly at 130s bpm, from then I decided to load her with a third pint of fluid and a fourth one, and what we noticed her dry lips and mucosa (tongue adhered with the lower lip and have to separate them and see if she was dehydrated and yes, she was indeed) - she was waking up frequently and managed by muscle relaxant and covered with analgesia, and our discussion with Attending, we suggested this patient was dehydrated - not well prepared, as in our practice at the ICU, we saw lots of patients with hypertension relieved by hydrating the patient with crystaloid - Physiology is remarkable.
We tried to reduce more the heart rate by administration of 0.2 mg of metoprolol every like 5 minutes to check response, and it was really helpful to reduce the heart rate to less than the ischemic threshold of 120 bpm.
Patient smoothly extubated on PSVPro and put her for 10 minutes on simple face mask, then was sent to the ward with SPO2 of 98% room air and pulse rate less than 100 !
Me, and the first PGY1 (discussion circle two days ago - I called her and told her that our discussion probably makes a difference today) and we agreed to monitor every next case of CS and to do this two hands technique to see, is it actually reduce the heart rate? If so, this will be another option, as I am thinking loudly to use it often to ensure good flow both at aotric vs inferior vena cava.
This is the picture of one hand vs two hand left tilting of the uterus.
Thanks to this PGY1, she saved a patient on her off day with her knowledge I learned from her from our discussion.
Thanks for reading!
I am open to learning as you know me, I hope that this will bring additional knowledge!
Best,
Sincerely,
Dr Amir Al Shimmarii
P. S. Quoted from one of the textbook:
During CPR; to improve the quality left uterine displacement is advocated to remove the aorto-caval compression. This is done manually by 1-hand or 2-hand technique or by using a wedge of predetermined angle.
I hope you are doing well, bringing up a case for discussion.
Yesterday we had an interesting case for C/S - elective, she was prepared, fasting time roughly over 8 hours, patient is young, and once she laid supine, her pulse rate was exceeding 150 bpm, and sometime reached 170 bpm. Very vague, isn't it? Aside from being covid positive! BP 130/80 like normal!
Well, we were skeptical between to proceed with neuraxial vs GA, we decided to do ECG, appears sinus tachycardia only.
Two days ago, we were having a discussion about aortocaval compression, and one of the methods especially used for CPR in pregnants, are to do either one hand or two hand left side tilt of abdomen, it helps in CPR. Actually, I requested from our primary PGY1 residents to aid the discussion, and interestingly one of the residents shows us a picture of the procedure, which is very interesting. (one hand vs two hands)
Back to the patient, while she was supine, I tried to do two hands pressure towards the left side, and what was amazingly happened, is that her pulse rate dropped to 135 bpm!
I freed my hand, the Tachycardia increased between 150 to 160 bpm.
We weren't sure, why? Our Attending was at the bedside instructing us, and then we put (pint of fluid - no wedge pillow available) underneath the right iliac crest to create left tilting, but wasn't that much successful to reduce the heart rate even with plus bed tilting, unless I put my both hands again, the pulse dramatically dropped to 130s bpm. Then we assumed it is an aortocaval compression, but why normotensive? It should've be hypotension, sweating,,, etc isn't it? Patient wasn't even anxious.
We ask the patient to sit, like we are trying to do spinal, her pulse rate dropped to 130s, once she was back supine, it increased very fast to 165 bpm!
I kept my hands on again and dropped to 130s not even 140s, then we decided GA, and another PGY1 started her induction smoothly, and with scoline - RSI, once scoline in, I felt my push was much better and stronger to get PR of 120 bpm, and she tubed the patient with ease!
The OBGYNs residents c/s her fast, reached the baby, but it was obstructed too, they got the help of their Senior, and I removed the pint of normal saline from underneath the patient, and once the baby out crying to life, we got a PR fixed on 135 bpm, and the patient didn't go hypotensive at all or hypoxic, except lax uterus and we managed it by decreasing the isoflurane + giving oxytocine, and the tachycardia kept interestingly at 130s bpm, from then I decided to load her with a third pint of fluid and a fourth one, and what we noticed her dry lips and mucosa (tongue adhered with the lower lip and have to separate them and see if she was dehydrated and yes, she was indeed) - she was waking up frequently and managed by muscle relaxant and covered with analgesia, and our discussion with Attending, we suggested this patient was dehydrated - not well prepared, as in our practice at the ICU, we saw lots of patients with hypertension relieved by hydrating the patient with crystaloid - Physiology is remarkable.
We tried to reduce more the heart rate by administration of 0.2 mg of metoprolol every like 5 minutes to check response, and it was really helpful to reduce the heart rate to less than the ischemic threshold of 120 bpm.
Patient smoothly extubated on PSVPro and put her for 10 minutes on simple face mask, then was sent to the ward with SPO2 of 98% room air and pulse rate less than 100 !
Me, and the first PGY1 (discussion circle two days ago - I called her and told her that our discussion probably makes a difference today) and we agreed to monitor every next case of CS and to do this two hands technique to see, is it actually reduce the heart rate? If so, this will be another option, as I am thinking loudly to use it often to ensure good flow both at aotric vs inferior vena cava.
This is the picture of one hand vs two hand left tilting of the uterus.
Thanks to this PGY1, she saved a patient on her off day with her knowledge I learned from her from our discussion.
Thanks for reading!
I am open to learning as you know me, I hope that this will bring additional knowledge!
Best,
Sincerely,
Dr Amir Al Shimmarii
P. S. Quoted from one of the textbook:
During CPR; to improve the quality left uterine displacement is advocated to remove the aorto-caval compression. This is done manually by 1-hand or 2-hand technique or by using a wedge of predetermined angle.
Last edited:

