- Joined
- Jan 14, 2006
- Messages
- 11,882
- Reaction score
- 20,915
Seems like a new world but not without its challenges. Would love some insights/opinions from those directly involved.
 www.nytimes.com
www.nytimes.com
FDA Approves World’s First Crispr Gene-Editing Drug for Sickle-Cell Disease
FDA Approves World’s First Crispr Gene-Editing Drug for Sickle-Cell Disease
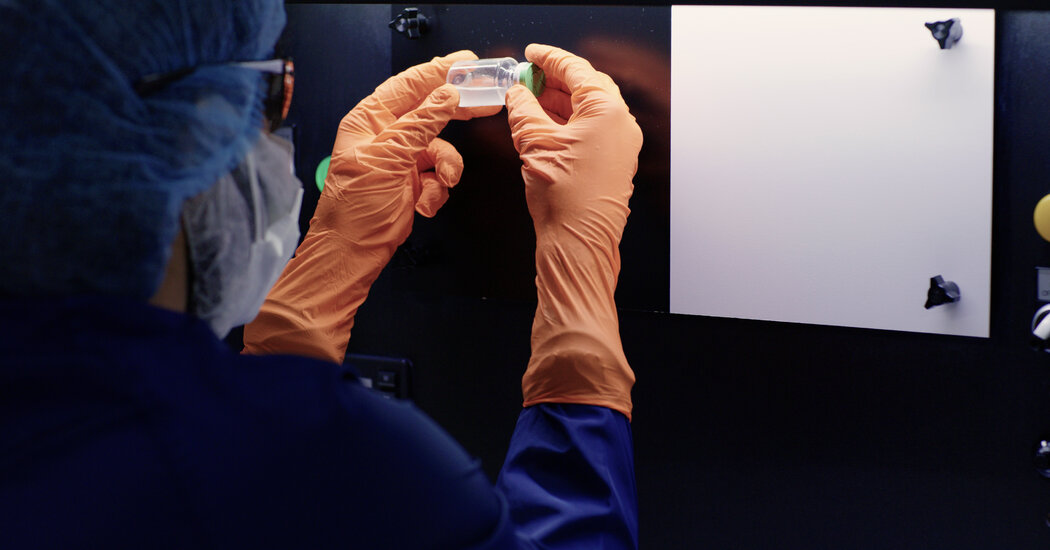
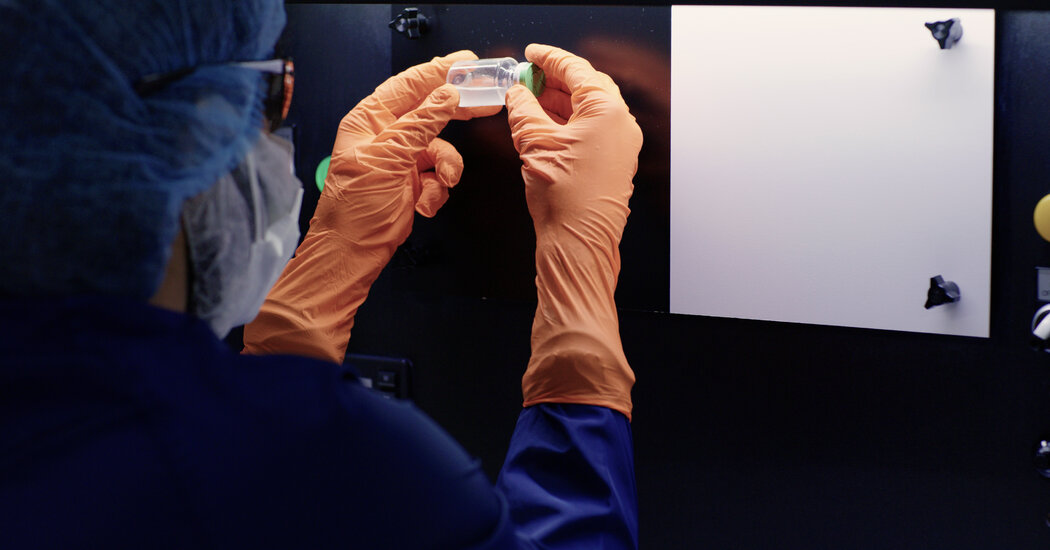
F.D.A. Approves Sickle Cell Treatments, Including One That Uses CRISPR
People with the genetic disease have new opportunities to eliminate their symptoms, but the treatments come with obstacles that limit their reach.
FDA Approves World’s First Crispr Gene-Editing Drug for Sickle-Cell Disease
FDA Approves World’s First Crispr Gene-Editing Drug for Sickle-Cell Disease
