- Joined
- Mar 27, 2011
- Messages
- 2,062
- Reaction score
- 2,798
You misunderstood me. My point is, failure to be notified of the option of an MD was not the reason this occurred. I'm obviously not a lawyer, but that doesn't seem like an incriminating piece of evidence.This is a young patient who is permanently disabled and will need expensive care for the remainder of what could still be a very long life. How much are good nursing homes nowadays? How much will it cost to provide 24/7 nursing care for 30-50yrs? How much will his medical bills be? And mom has relocated to take care of her son. What did she do for a living? What did the patient do before his injury? Economic damages can be huge.
Tort reform states have caps on noneconomic damages (like pain and suffering) but there are no limits on economic damages. California is a tort reform state with a cap of $250k for noneconomic damages. However, there have been 8 figure settlements and jury awards when a child or young professional becomes permanently disabled by malpractice. When a patient dies, the settlements tend to be smaller. But when they survive and need lifetime care, the amounts can be very high.
Edit:
In rereading the article, it says $8mil of the award was for medical care. Of the remaining $13mil, I’m sure some of it was for lost income, some for pain and suffering, and some to send a message.
That's like me going to dinner and not being told that there's an option to have a chef or an associate prepare my food. Except the associate serves me raw chicken because he put it in the oven, didn't turn the oven on and then covered it with gravy to make it appear cooked while taking a 12 minute smoke break.
The incriminating piece here isn't my failure to be notified. It's the ******* associate.
If anyone has this and can share, I would sincerely appreciate it.
Anesthesiologist Staffing Ratio and Surgical Patient Morbidity and Mortality
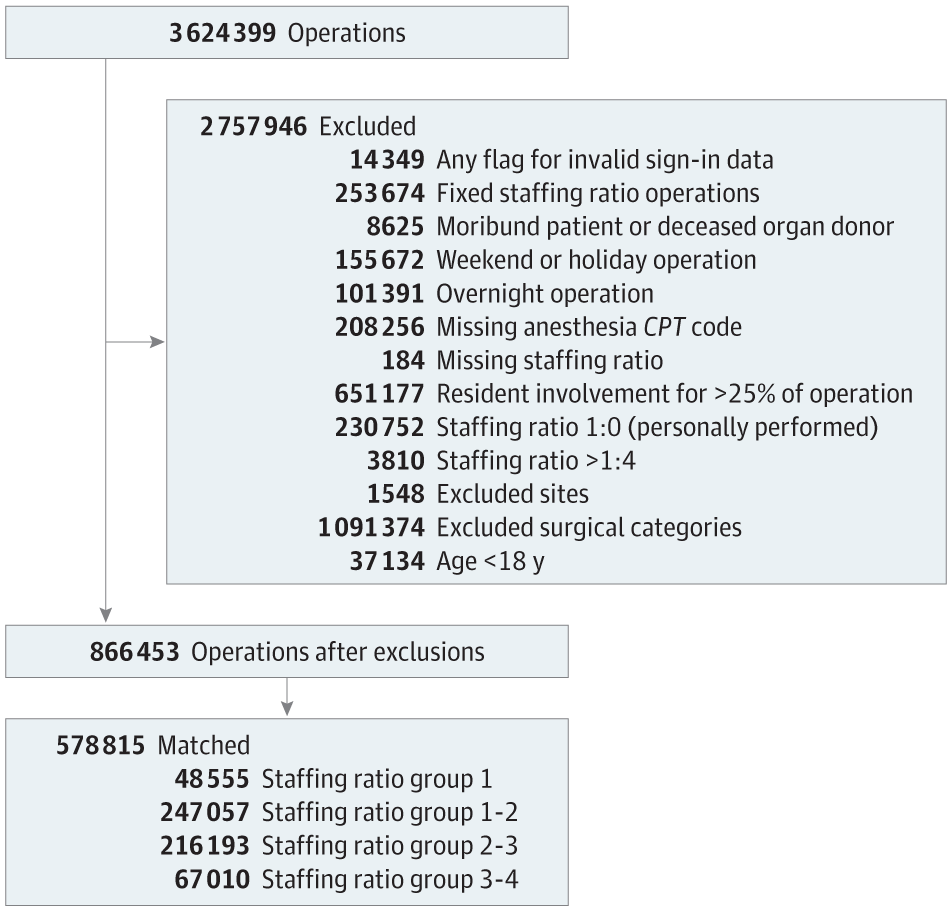
This cohort study uses data from the Multicenter Perioperative Outcomes Group database to examine the association between intraoperative anesthesiologist staffing ratio and surgical patient morbidity and mortality across 23 hospitals in 18 states.

