On my drug interaction checker (YouScript), I have had stop sign warnings (the highest level of warning) for anticholinergic drugs I take for a couple of years now, whereas before there were no warnings for them. Other drug checkers give no warning about this interaction whatsoever. The nice thing about this checker is that it rates the evidence and gives links to the research they use.
This is what it says:
"
- Increased risk of constipation, dry mouth, cognitive impairment, confusion and urinary retention.
- Avoid combinations of highly anticholinergic drugs if possible."
Combinations of Medium/High Anticholinergic Activity Drugs [my drug names—deleted]
Effects
Mechanism: Additive anticholinergic effects.
Combinations of medications with anticholinergic properties may cumulatively increase the risk for adverse peripheral anticholinergic effects such as constipation, urinary retention, dry mouth and dry eyes as well risk for central anticholinergic effects such as confusion, cognitive dysfunction and delirium.
1,
2
Several scales recognized by the Beers Criteria such as the Anticholinergic Risk Scale (ARS) and the Anticholinergic Drug Scale (ADS) stratify the degree of anticholinergic burden conferred by individual medication.
2
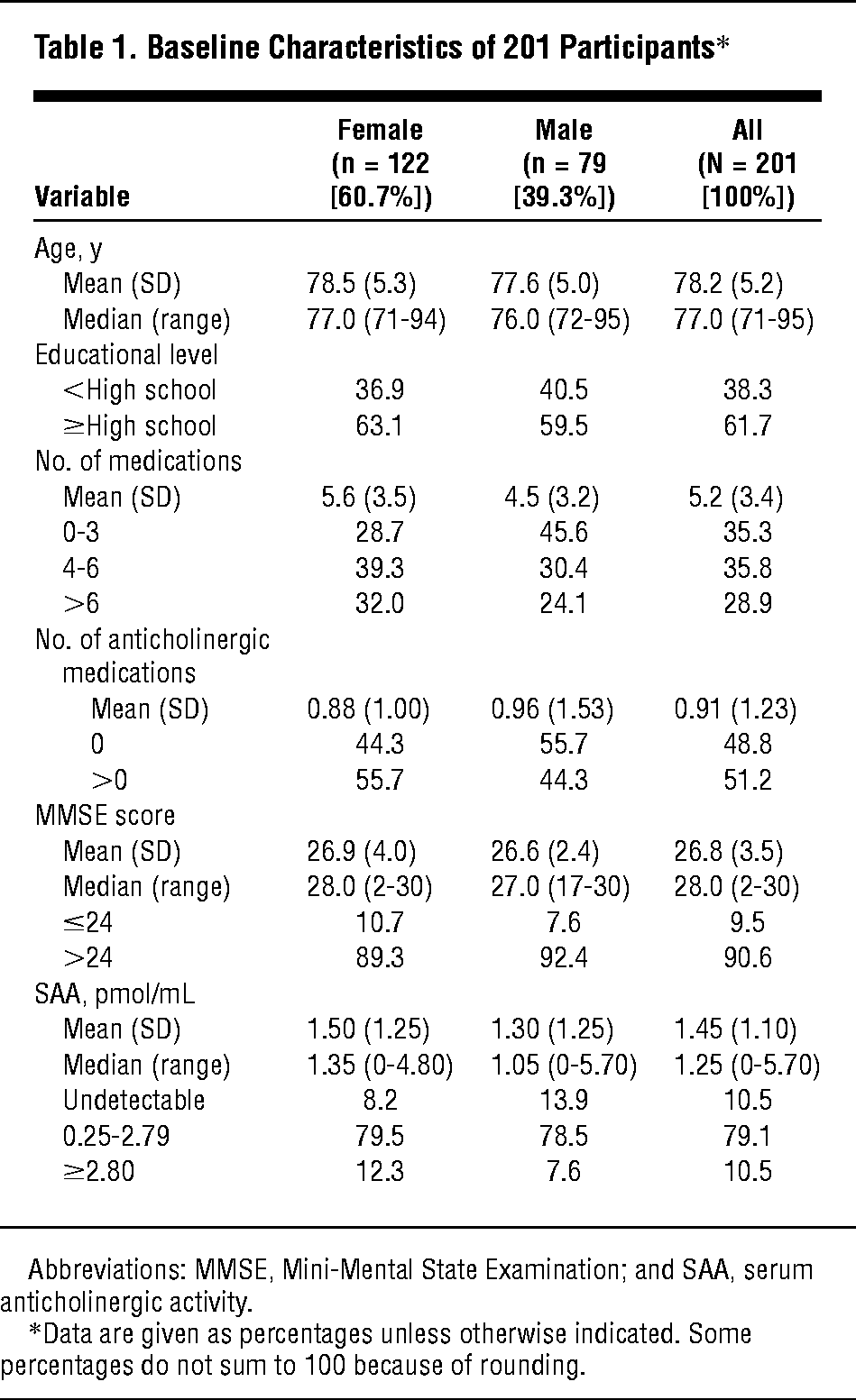
Research is ongoing. Studies assessing increasing anticholinergic medication burden utilizing the ARS, ADS and other scales have found significantly increased risk for worsened functional outcomes, institutionalization and even mortality, while other studies have not shown statistically significantly worsened outcomes or mortality.
3
Management
Avoid combinations of highly anticholinergic drugs if possible. Weigh risk versus benefit of each medication. Consider use of alternative medication(s) with lower anticholinergic activity if possible and when clinically appropriate.
Monitor for increased risk of adverse anticholinergic adverse effects such as constipation, urinary retention, dry mouth, dry eyes, confusion and cognitive dysfunction.
Evidence: Moderate

 www.cnn.com
www.cnn.com