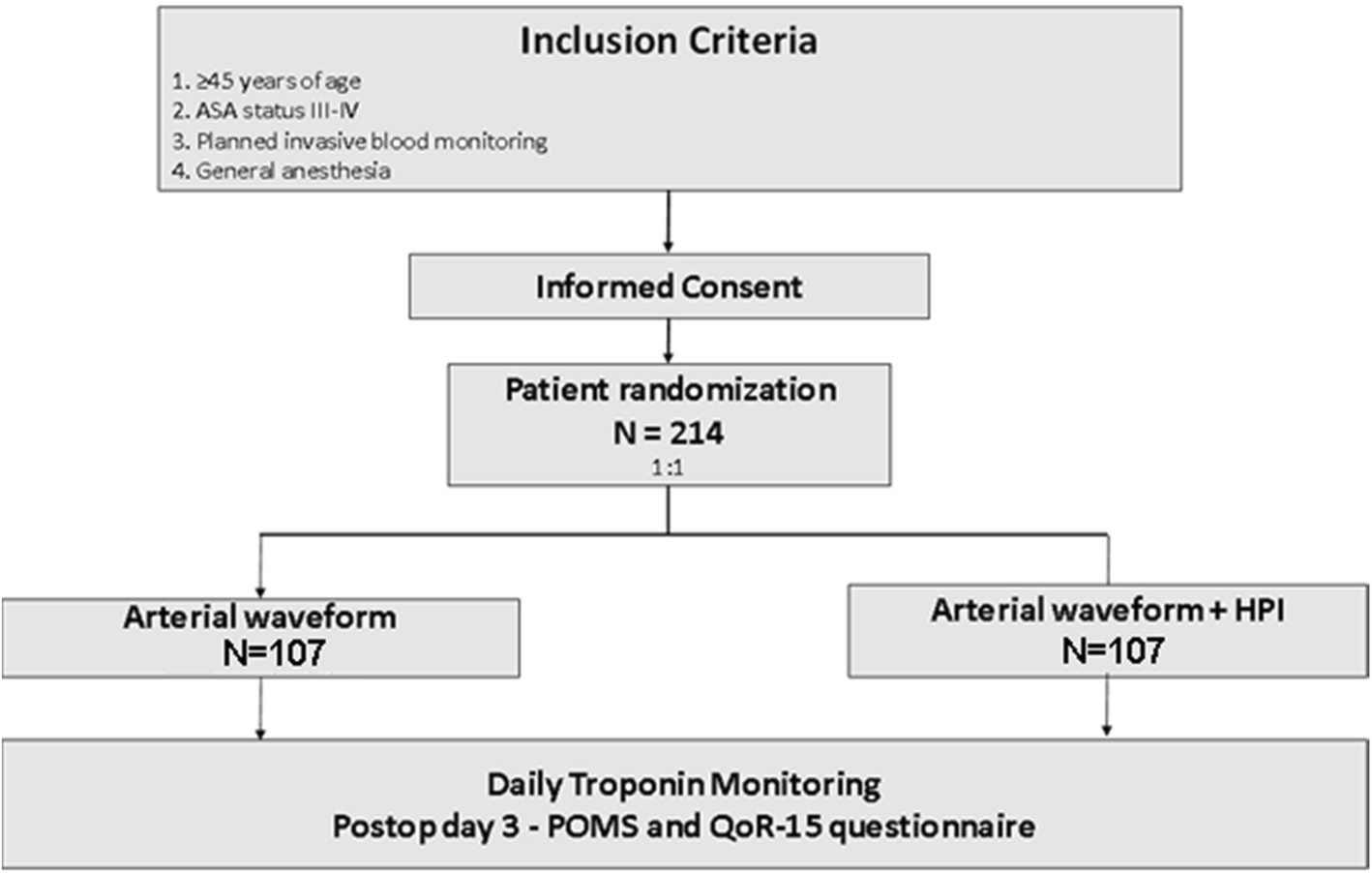
We have a decently busy ortho trauma service at my shop, and we do a lot of hip fractures on the typical old/frail people falls. Apparently the trauma Service at my hospital has had issues with patients being under-resuscitated while in the hospital (they’ve been trending lactates during their stay to determine this). Now the trauma service has requested we apply the Edwards clearsite on ALL hip Fx surgeries and resuscitate with a goal directed approach using the clearsite SVV as guidance.
My personal experience with this device is poor. Seems to fail frequently and/or give unreliable data. Maybe I’m just cursed and have bad luck. Anyone use it regularly for this, or have any thoughts on mandating it for all hip fix surgeries?
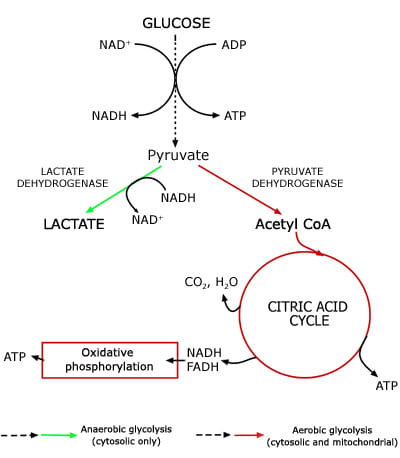
As a CV anesthesiologist, if I’m truly worried about CO, resuscitation, and Hemodynamic monitoring I’ll use a traditional A-line (utilizing SPV, PPV, ABGs, lactates), quick preop/post-op TTEs that I do myself, and Intraop TEE in really fragile patients. But a lot of my partners either aren’t comfortable with that or don’t want to do it, hence this blanket policy to use clearsite.
My personal experience with this device is poor. Seems to fail frequently and/or give unreliable data. Maybe I’m just cursed and have bad luck. Anyone use it regularly for this, or have any thoughts on mandating it for all hip fix surgeries?
As a CV anesthesiologist, if I’m truly worried about CO, resuscitation, and Hemodynamic monitoring I’ll use a traditional A-line (utilizing SPV, PPV, ABGs, lactates), quick preop/post-op TTEs that I do myself, and Intraop TEE in really fragile patients. But a lot of my partners either aren’t comfortable with that or don’t want to do it, hence this blanket policy to use clearsite.