Barry1960
New Member
- Joined
- Feb 13, 2024
- Messages
- 2
- Reaction score
- 1
I have an ethical dilemma that I need help with.
I am an Endocrinologist, who lives in a neighboring state to my sister and mother. I am DPoA for medical affairs for my 90 year old mother with moderate Alzheimer’s Disease. My sister, who my mother lives with, is DPoA for finances and pays the bills. My mother has both Medicare part A and B and Federal Blue Cross Insurance. She fell, fracturing her pelvis through the right acetabulum (and ilium), which was repaired surgically. She is non-weight bearing for 12 weeks and as result is in a nursing/rehab facility, rather than my sister’s home until she can walk again.
The issue: My sister shows me bills to Blue Cross from a Physical Medicine physician assistant at the rehab facility for 4 visits per week for my mother’s first 7 weeks, while she was on SNF status, with copays of $25/visit (in 2023) and $30/visit (for 2024). There were no charges for visits starting the day after SNF was stopped and we began nursing home self pay.
My mother was stable the entire time (expect for minimally symptomatic COVID) and in my opinion, did not need 4 provider visits per week X 7 weeks. After a visit with the nursing home director, I was told the PA would call me to talk about it. Instead I was called by her supervisory physician, who tells me the PA is off due to a death in the family. He does not acknowledge anything wrong with the billing but agrees to contact his team and refund my mother’s co-pays.
Am I making a mountain out of a molehill? Do I have a responsibility to take this matter further to protect the public from what is at a minimum over-charging and possibly might even be outright fraud. If so, should I go to the facility director, the state medical society, Medicare, Blue Cross or some combination of the above?
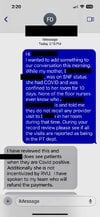
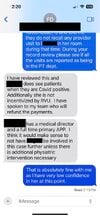
The screen shots below are text messages from my phone that conclude my interaction with the supervising Physiatrist.
I am an Endocrinologist, who lives in a neighboring state to my sister and mother. I am DPoA for medical affairs for my 90 year old mother with moderate Alzheimer’s Disease. My sister, who my mother lives with, is DPoA for finances and pays the bills. My mother has both Medicare part A and B and Federal Blue Cross Insurance. She fell, fracturing her pelvis through the right acetabulum (and ilium), which was repaired surgically. She is non-weight bearing for 12 weeks and as result is in a nursing/rehab facility, rather than my sister’s home until she can walk again.
The issue: My sister shows me bills to Blue Cross from a Physical Medicine physician assistant at the rehab facility for 4 visits per week for my mother’s first 7 weeks, while she was on SNF status, with copays of $25/visit (in 2023) and $30/visit (for 2024). There were no charges for visits starting the day after SNF was stopped and we began nursing home self pay.
My mother was stable the entire time (expect for minimally symptomatic COVID) and in my opinion, did not need 4 provider visits per week X 7 weeks. After a visit with the nursing home director, I was told the PA would call me to talk about it. Instead I was called by her supervisory physician, who tells me the PA is off due to a death in the family. He does not acknowledge anything wrong with the billing but agrees to contact his team and refund my mother’s co-pays.
Am I making a mountain out of a molehill? Do I have a responsibility to take this matter further to protect the public from what is at a minimum over-charging and possibly might even be outright fraud. If so, should I go to the facility director, the state medical society, Medicare, Blue Cross or some combination of the above?
The screen shots below are text messages from my phone that conclude my interaction with the supervising Physiatrist.
Attachments
Last edited: