Promoting prostate HDR in US would not be bad.
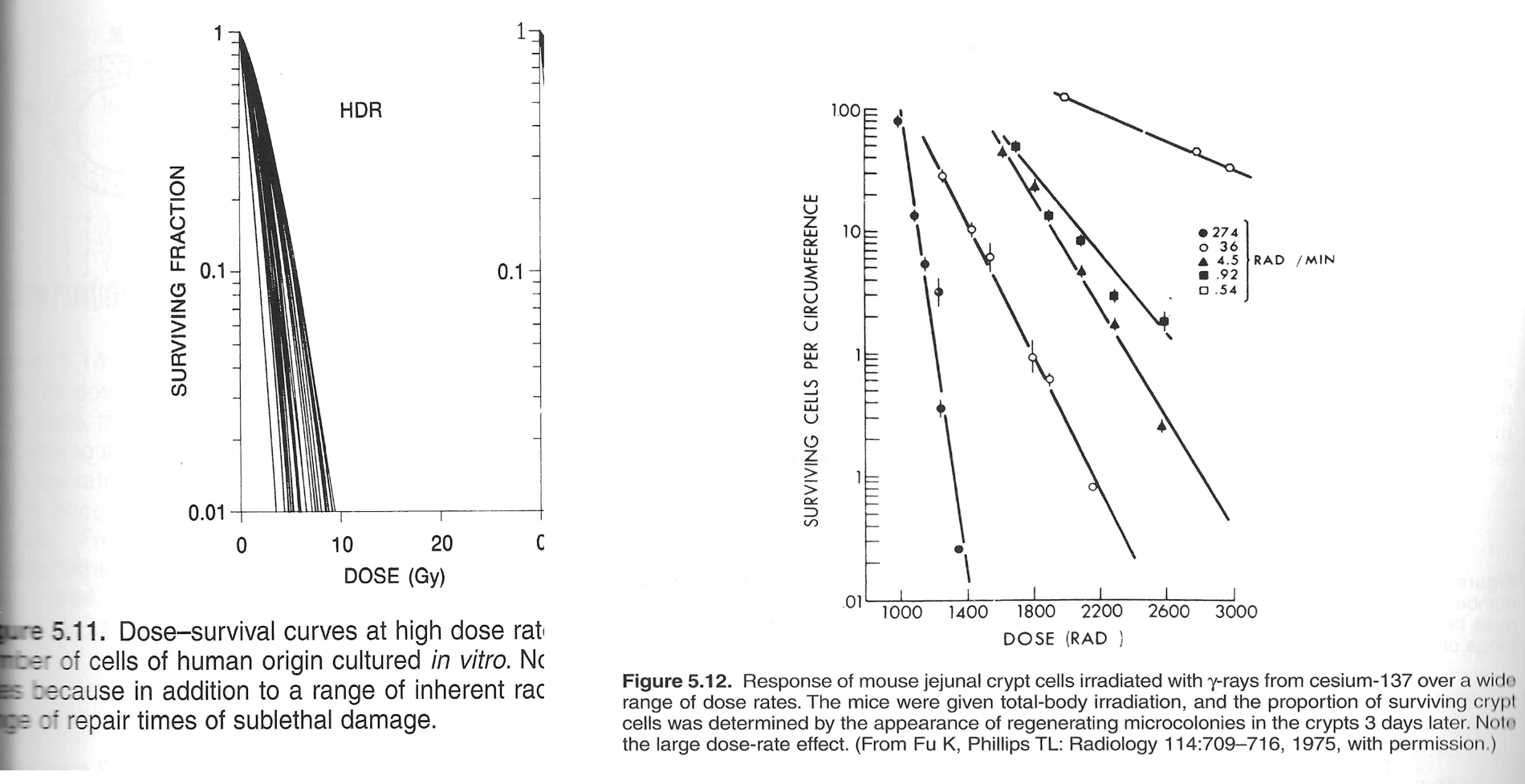
In theory based on this chart could single fraction prostate HDR pay $23K global? If so look out for a prostate HDR renaissance in the US. CMS is, wittingly or unwittingly, massively incentivizing (and disincentivizing) certain treatment paradigms with this new model. For better or worse!