- Joined
- Apr 6, 2013
- Messages
- 872
- Reaction score
- 448
What would you do????
34yo F
BL buttock type pain radiating to lateral thighs stopping at the knees. No neuropathic descriptors.
Has failed SIJ, MBB, ESI with different provider. Saw a surgeon who did not recommend surgery.
Exam pos for BL SIJ TTP and + Fabers. Groin pain with hip ER BL. Low back somewhat diffusely TTP.
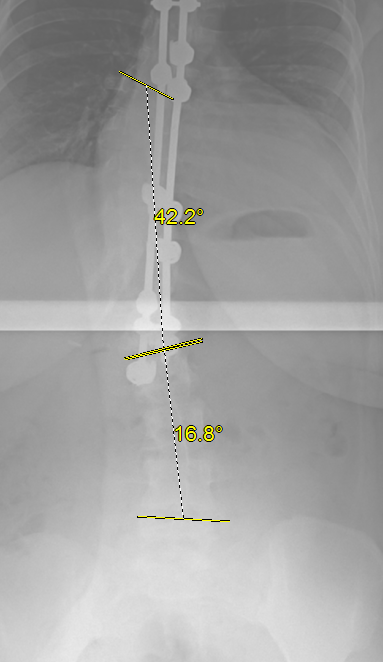
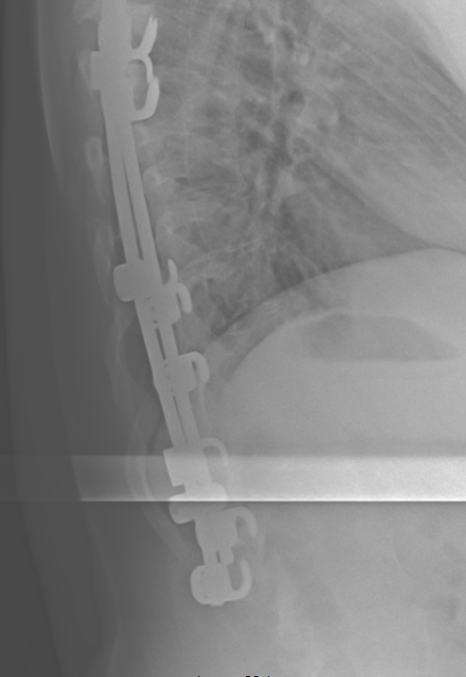
H/o large thoracolumbar scoliosis correction procedure with Harrington rods/hooks as a pre-teen
Rads read is Osteitis condensans ilii and hips normal

MRI report low back
FINDINGS: There is a levoscoliosis of the lumbar spine with a rotatory
component. There are rods in the thoracic spine extending to the
thoracolumbar junction on prior x-ray. This results in some metal artifact
on the current exam. Lumbar vertebral body heights appear maintained. There
is minimal narrowing of the L3-4 and L5-S1 discs. There is a hemangioma at
L2 and L3. The conus is obscured by metal artifact.
T12-L1 and L1-2: There is no disc protrusion. No central or neural
foraminal stenosis is seen. Metal artifact somewhat obscures the central
canal.
L2-3: There is no disc protrusion, or central or neural foraminal stenosis.
L3-4: There is no disc protrusion or central or neural foraminal stenosis.
Minimal right facet degenerative change is present.
L4-5: There is no disc protrusion or central or neural foraminal stenosis.
Mild facet degenerative change is present.
L5-S1: There is a small midline annular fissure, without disc protrusion or
central or neural foraminal stenosis. Mild facet degenerative change is
present.
IMPRESSION: Scoliosis, with mild facet degenerative change, as above. There
is a small midline annular fissure at L5-S1.
I did cymbalta, mobic, PT (because she was tight everywhere with poor flexibility and inactive). Seems like she will fail this stuff though as she has done PT in the past.
34yo F
BL buttock type pain radiating to lateral thighs stopping at the knees. No neuropathic descriptors.
Has failed SIJ, MBB, ESI with different provider. Saw a surgeon who did not recommend surgery.
Exam pos for BL SIJ TTP and + Fabers. Groin pain with hip ER BL. Low back somewhat diffusely TTP.
H/o large thoracolumbar scoliosis correction procedure with Harrington rods/hooks as a pre-teen
Rads read is Osteitis condensans ilii and hips normal
MRI report low back
FINDINGS: There is a levoscoliosis of the lumbar spine with a rotatory
component. There are rods in the thoracic spine extending to the
thoracolumbar junction on prior x-ray. This results in some metal artifact
on the current exam. Lumbar vertebral body heights appear maintained. There
is minimal narrowing of the L3-4 and L5-S1 discs. There is a hemangioma at
L2 and L3. The conus is obscured by metal artifact.
T12-L1 and L1-2: There is no disc protrusion. No central or neural
foraminal stenosis is seen. Metal artifact somewhat obscures the central
canal.
L2-3: There is no disc protrusion, or central or neural foraminal stenosis.
L3-4: There is no disc protrusion or central or neural foraminal stenosis.
Minimal right facet degenerative change is present.
L4-5: There is no disc protrusion or central or neural foraminal stenosis.
Mild facet degenerative change is present.
L5-S1: There is a small midline annular fissure, without disc protrusion or
central or neural foraminal stenosis. Mild facet degenerative change is
present.
IMPRESSION: Scoliosis, with mild facet degenerative change, as above. There
is a small midline annular fissure at L5-S1.
I did cymbalta, mobic, PT (because she was tight everywhere with poor flexibility and inactive). Seems like she will fail this stuff though as she has done PT in the past.
