Where do you guys routinely put your needle tip when performing your interscalene blocks? I've read resources that say multiple conflicting things:
-"Needle aimed in between nerve roots instead of directly at them in order to minimize risk of accidental nerve injury" (Nysora). But then the same resource goes on to say
"It is prudent to avoid injecting between the nerves coming from a single root, as this may result in an intraneural injection"
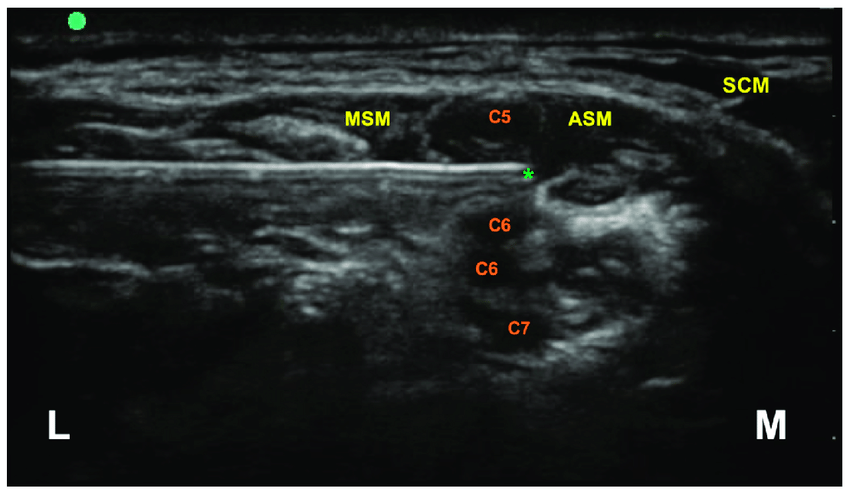
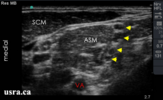
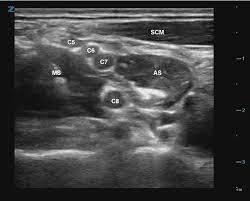
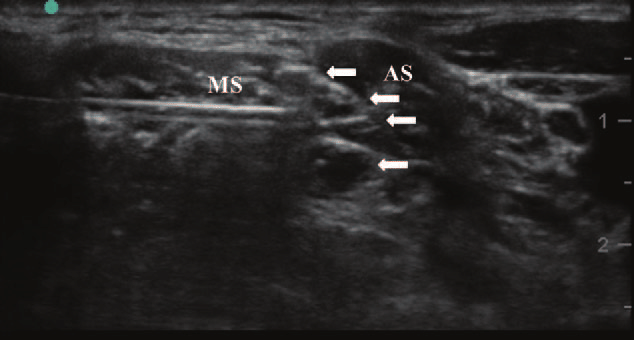
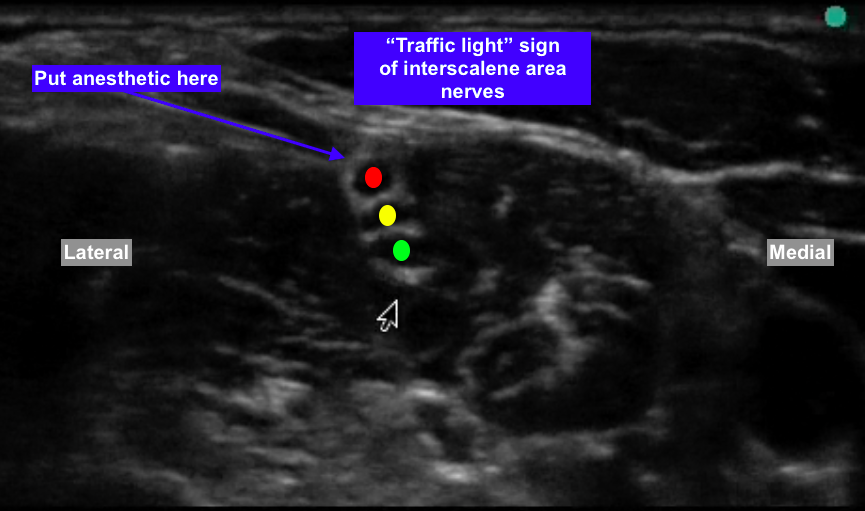
So when you are looking at 3-5 black circles in the interscalene groove, how do you differentiate which ones are C5, C6, C7 vs. multiples coming off the same root? For example how do we know in the picture below that we are not looking at C5, C6, C6, C7 (or any other anatomical variant).
Or do you simply inject tangential to the posterior border of the cluster of 3 "stoplights"?
Or do you inject tangential to the superior border of the cluster? In my mind this is incorrect because superior deposition I think will likely lead to anterior spread and increased phrenic nerve blockade.
-"Needle aimed in between nerve roots instead of directly at them in order to minimize risk of accidental nerve injury" (Nysora). But then the same resource goes on to say
"It is prudent to avoid injecting between the nerves coming from a single root, as this may result in an intraneural injection"
So when you are looking at 3-5 black circles in the interscalene groove, how do you differentiate which ones are C5, C6, C7 vs. multiples coming off the same root? For example how do we know in the picture below that we are not looking at C5, C6, C6, C7 (or any other anatomical variant).
Or do you simply inject tangential to the posterior border of the cluster of 3 "stoplights"?
Or do you inject tangential to the superior border of the cluster? In my mind this is incorrect because superior deposition I think will likely lead to anterior spread and increased phrenic nerve blockade.
Attachments
Last edited: