I think you’re right ESE. On the other hand, since most of the toxicity comes from cheat wall, if you’re treating it seems easy enough to include some of the axilla. If we did more IMRT we would be more creative about how much we treated
Ah yeah good point - for me, "chest wall alone" takes a pretty good piece of axillary levels depending on how things shake out. No routine bolus or boost (case by case, never say "never" or "always"). Axilla is basically unavoidable with 3D. Now, if/when we move into more IMRT, that's an interesting debate.
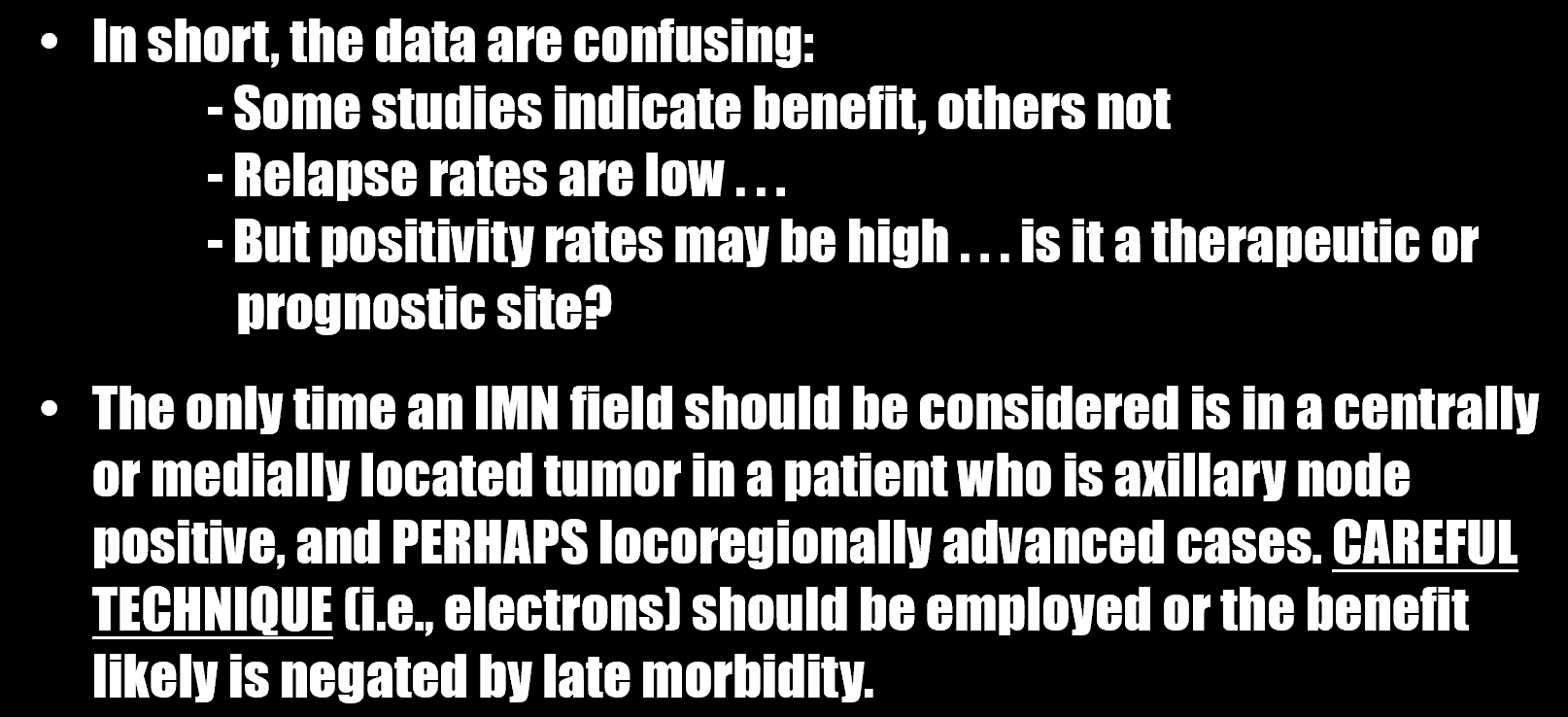
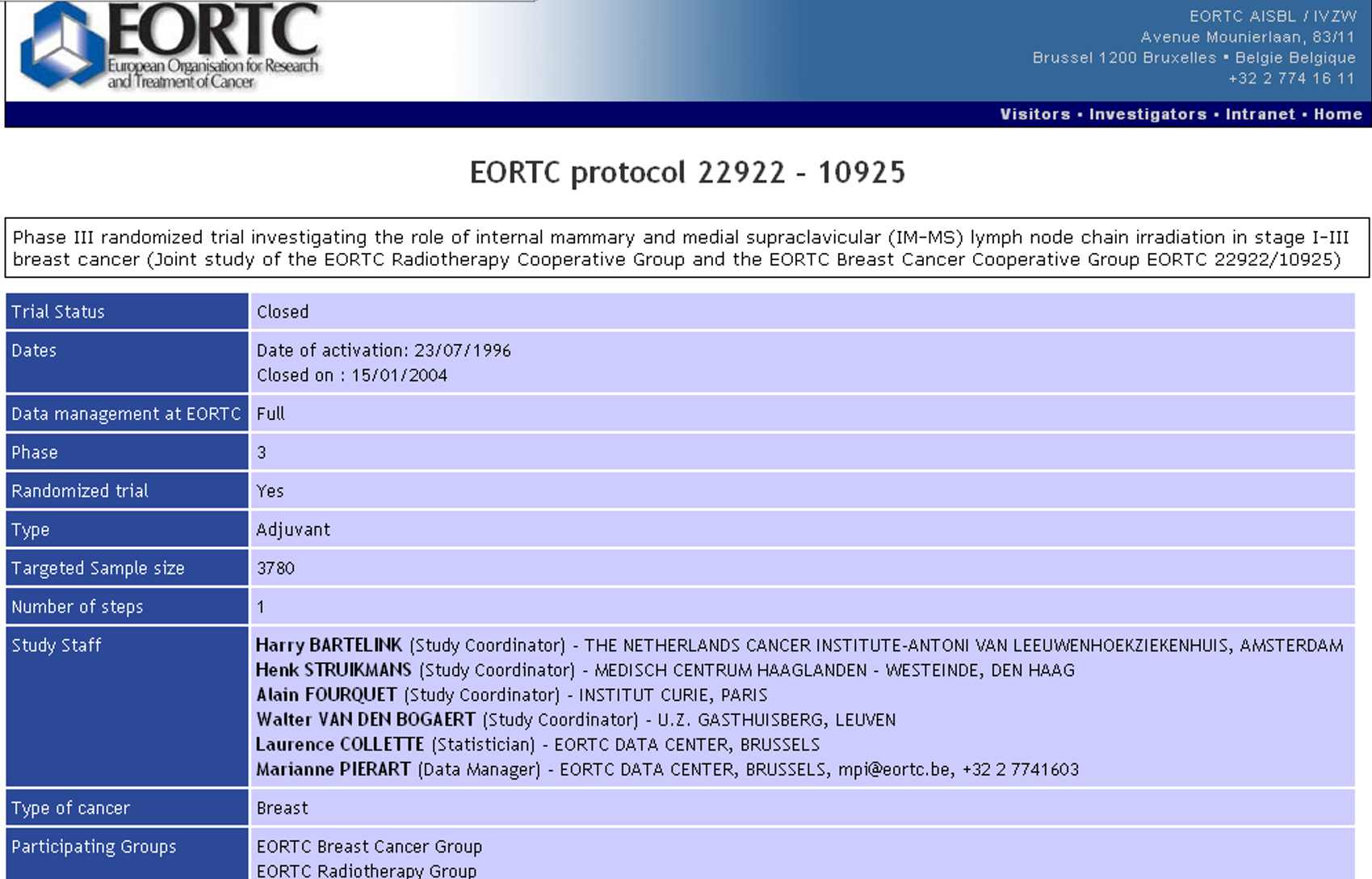
I got very frustrated trying to lock down "how do you define RNI" a few years ago because it's (obviously) not universally defined. For me, nowadays, RNI means the whole shebang: SCV, I/II/III, and IMNs. Sometimes I name things "Rotter's nodes" if I want to get a lot of eye rolls.
I guess, here, it depends more on where you draw your superior border. Near as I can tell, down the rabbit hole, the "official" definition for high tangents is "within 2cm of the humeral head". Which...meh, that depends on the height of the person.
Sushil and crew published a paper in PRO in 2018 or so about UPMC trying to standardize the whole Z11/ALND omission thing across the network. Their version of "high tangents" includes explicitly contouring Levels I and II.
So...reflecting on the internal struggle I face in this q3 month contouring adventure, I guess my PTV does include I/II/III, more or less. I don't (or at least haven't) gone out of my way to go up to the coracoid process like I would doing Z11/UPMC "high tangents" style cases.
This is all somewhat pedantic if you're doing 3D anyway, and depends on the skill of your Dosimetry and the body habitus of the patient. Especially because breast/MA20 has the magical "80% IDL" thing.
Thinking about this really rustles my jimmies, because the breast academicians sure draw some hard lines in the sand over topics that have NOT been exhaustively interrogated.