- Joined
- Aug 8, 2013
- Messages
- 172
- Reaction score
- 32
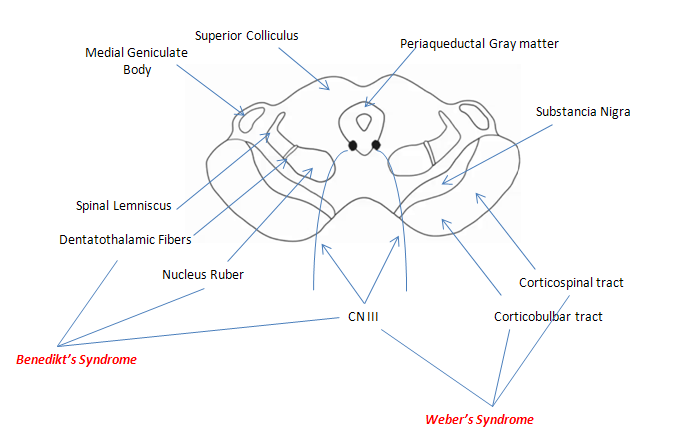
A 80 year old man was observed to have an episode of loss of consciousness. Upon awakening he complained of double vision and there was a notable tremor in his left arm. There was a mildly elevated blood pressure. Mental status was good and speech was articulate and appropriate. With the eyelids retracted the right eye had a dilated pupil and a lateral strabismus. On attempted lateral gaze to the left the right eye would not proceed across the midline. The right pupil did not constrict in either the direct or consensual pupillary light reflexes. Hearing was normal as were cranial nerves 5 through 12. Pain and temperature sensation from the face and body was normal bilaterally. Proprioception and vibratory sense on the right side of the body was normal but was diminished on the left. Muscle strength on the left was slightly diminished and deep tendon reflexes were slightly increased. There was no Babinski sign. The finger-to-nose test was normal on the right but the left arm showed an intention tremor and dysmetria. There were occasional involuntary movements of the left arm. What is the most likely diagnosis?
A) Dorsal midbrain syndrome
B) Paramedian midbrain syndrome
C) Lateral medullary syndrome
D) Medial medullary syndrome
E) Facial colliculus syndrome
F) Medial longitudinal syndrome
Show your thought process please.
A) Dorsal midbrain syndrome
B) Paramedian midbrain syndrome
C) Lateral medullary syndrome
D) Medial medullary syndrome
E) Facial colliculus syndrome
F) Medial longitudinal syndrome
Show your thought process please.