I'm currently applying to med school and I have been shadowing a Family Medicine doctor.
A 49 y/o male came in for his first doctor's visit in over 10 years. He looked totally normal and healthy, but BMI was maybe 28.
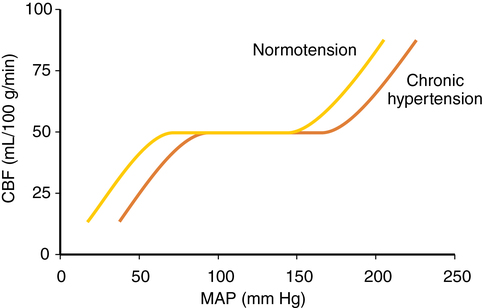
His blood pressure was 205 / 130 mmHg, roughly. The doctor took a few readings to see if it would go down as he remained seated and motionless, but it did not.
How common is this? I mean, I thought a systolic above 180 mmHg was considered an emergency. This guy got sent home with a scrip for chlorthalidone, advice to come back soon (which honestly wasn't worded that strongly), and also a prediction that he would need to have a second antihypertensive agent added at the next visit.
This guy had no symptoms at all. He came in because his wife was hounding him about his 50th birthday. The big Five-Oh. He's not immortal anymore.
How high does blood pressure get in people who are asymptomatic? Have you seen higher?
How high does blood pressure go during a cocaine or methamphetamine overdose? Or maybe a pheochromocytoma?
A 49 y/o male came in for his first doctor's visit in over 10 years. He looked totally normal and healthy, but BMI was maybe 28.
His blood pressure was 205 / 130 mmHg, roughly. The doctor took a few readings to see if it would go down as he remained seated and motionless, but it did not.
How common is this? I mean, I thought a systolic above 180 mmHg was considered an emergency. This guy got sent home with a scrip for chlorthalidone, advice to come back soon (which honestly wasn't worded that strongly), and also a prediction that he would need to have a second antihypertensive agent added at the next visit.
This guy had no symptoms at all. He came in because his wife was hounding him about his 50th birthday. The big Five-Oh. He's not immortal anymore.
How high does blood pressure get in people who are asymptomatic? Have you seen higher?
How high does blood pressure go during a cocaine or methamphetamine overdose? Or maybe a pheochromocytoma?