Semantics, Misnomer, or Uncertainty: Where Is the Epineurium on Ultrasound?
Endersby, Ryan MD, FRCPC; Albrecht, Eric MD, DEAA; Perlas, Anahi MD, FRCPC; Chan, Vincent MD, FRCPC
Regional Anesthesia and Pain Medicine . 37(3):360–361, May/June 2012.
doi: 10.1097/AAP.0b013e318253b48f
Author Information
Department of Anesthesia and Pain Medicine Toronto Western Hospital University Health Network University of Toronto Toronto, Ontario, Canada
Accepted for Publication: 29 February 2012
To the Editor:
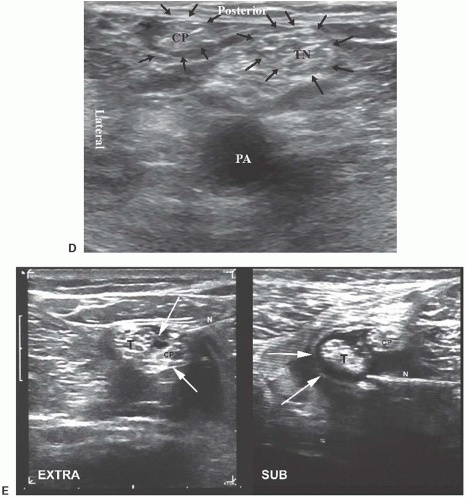
We read with interest the excellent study by Tran et al,1 showing that a single "subepineural" injection at the bifurcation of the sciatic nerve in the popliteal fossa is associated with a higher success rate and a shorter performance time than separate injections around the tibial and peroneal nerve divisions. They described the injection below a common sheath as subepineural. However, we would like to suggest that whether this layer represents a true epineurium or a separate adventitial layer or common sheath external to the epineurium is a matter of debate.2 The study by Vloka et al, which was quoted to support the conclusion of Tran et al that the injections were subepineural, was strictly an anatomic study with no correlation to ultrasound images.3 Vloka et al studied the anatomy of the sciatic nerve bifurcation in cadavers, and they in fact described the presence of multiple "epineural" layers. An inner epineural layer was identified, which they called the "interfascicular epineurium," extending between nerve fascicles, while a second tissue layer that surrounds the entire nerve was called the "epifascicular epineurium." In addition, a third loose connective tissue layer was identified external to the epineurium and was referred to as the "adventitia of the nerve."
Judging by the images presented in the study by Tran et al, it is unclear to us whether the "subepineural" injection refers to the interfascicular epineurium, the epifascicular epineurium, or possibly an injection deep into the adventitial layer but outside the epineurium of the 2 individual nerves themselves. Furthermore, there is a substantial amount of animal and human evidence that suggests subepineural (ie, intraneural) injections are usually accompanied by some degree of nerve swelling.4–6 In contrast, Tran et al stated that neural swelling was specifically avoided in both study groups. We believe that their images and the absence of neural swelling are both consistent with an injection outside the epineurium (possibly deep to the adventitial layer of the nerve) rather than a true subepineural injection.
In our opinion, this is an important matter and not just a matter of semantics. There is currently a heated debate in our specialty about the relative safety (or lack thereof) of intraneural injections. We should collectively strive to use common and clear terminology as to what constitutes intraneural (subepineurial) injection and what does not. We believe that Tran et al described a highly effective approach to block the sciatic nerve at its bifurcation that does not involve intraneural injection, as the title of the article would suggest.
Future studies that correlate sonographic images with anatomic findings at the level of the sciatic nerve bifurcation may shed more light on this issue.
Ryan Endersby, MD, FRCPC
Eric Albrecht, MD, DEAA
Anahi Perlas, MD, FRCPC
Vincent Chan, MD, FRCPC
Department of Anesthesia and Pain Medicine
Toronto Western Hospital
University Health Network
University of Toronto
Toronto, Ontario, Canada
Editor's Note: Thank you, Drs. Endersby et al and Tran et al, for commenting on this important issue. Readers should be aware that a study directly related to this issue will be published in the near future.