You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Love the credentials of the expert
D
deleted1180461
Are they providing the popcorn or do I have to bring my own?
- Joined
- Jun 21, 2022
- Messages
- 1,350
- Reaction score
- 4,541
And the almost uniform response of SDN so far is to take a **** on them?
I have to be honest. I feel like Rad Onc is taking a **** on me. Just tell me why I should be excited about BgRT like in terms of benefit for patients, or efficiency, really anything other than it is new and pays more than regular SBRT. I've asked the CMO and even invited him on the show. No dice (so far).
Maybe this is asking too much. I dont know.
Maybe I should stand there, covered in ****, and just let a nurse tell me how to treat my patients with lung cancer.
- Joined
- Jan 15, 2020
- Messages
- 45
- Reaction score
- 76
I can barely get 3D covered for bone Mets with extraosseous extension and yet Evicore is ready to approve bgrt?
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
They almost certainly won’t approveI can barely get 3D covered for bone Mets with extraosseous extension and yet Evicore is ready to approve bgrt?
But Medicare will, and then suddenly Medicare becomes a very lucrative payor for BgRT acquirers
New radiation device company dripping with pharma dollars that went through the trouble of getting their own specific (temporary) code. I'm sure they're doing easy stuff right now, likely at the request of their physics team, before trying more complicated things like mobile tumors in the lung, liver, etc, or more experimental stuff like hypoxic dose escalation for HN or what have you. But I don't doubt it's coming.
Sure this is twitter hype for the uninitiated, but that's the audience. If Terry is smart, and I'm sure he is, he'll be parading every rad onc naive hospital admin through over the next 6 months so they can "see the magic". And then hopefully squeeze ever more dollars and resources out of the COH bean counters.
And the almost uniform response of SDN so far is to take a **** on them? This stuff isn't a danger to private practice. My patients aren't gonna get on a plane for this. But if any of reflexion tech ultimately works and we treat more patients because of it, then only good for the field. Or we can turtle up and get buried by systemics in a self-fulfilling prophecy?
I'm going to freely take a **** on them because, in marketing their product, they completely misrepresent what we can and do accomplish as radoncs on a daily basis. PET fusion --> treatment has been around for well more than a decade. Yes, this machine could potentially increase throughput for SBRT patients with multiple mets. That's about it as far as I can tell.
It is, in fact, a danger to private practice, because these large, well-reimbursed academic centers who can afford to "invest" in technology such as this will use this machine as yet another marketing tool to suggest community radoncs aren't delivering world-class care. Additionally, instead of national radonc voices and "leaders" working on what would be valuable- improving the media/layperson perspective of radiation, helping other specialties understand where we are being underutilized, expanding indications for benign conditions, working on radiopharm- they're captured by industry and are working for them to market their machine.
- Joined
- Nov 2, 2019
- Messages
- 3,601
- Reaction score
- 14,885
Don't forget the sequel paper(s) where a group of authors (all with relevant COI people choose to ignore) do some crazy voodoo math where they invoke the cost of recurrence (inpatient stay, OR time, time off from work due to stress, etc) and arrive at the conclusion that ACTUALLY, IF YOU DO THE MATH, THE INCREASED COST OF BGRT FOR ROUTINE BREAST TREATMENT IS TOTALLY WORTH IT YOU GUYS.Can’t wait for the first paper to use reflexion to help outline the lumpectomy cavity
- Joined
- Sep 7, 2014
- Messages
- 3,566
- Reaction score
- 6,542
can I bill for bgRT if I match the sclerotic bone metastasis on CBCT to the slerotic bone metastasis on planing scan daily?
D
deleted1180461
Forget about doing a cone beam, I can’t even bill for 3D to treat a sclerotic bone met, so I’m going to go with no. I’m surprised we can even still ct sim them at this point.can I bill for bgRT if I match the sclerotic bone metastasis on CBCT to the slerotic bone metastasis on planing scan daily?
- Joined
- Sep 7, 2014
- Messages
- 3,566
- Reaction score
- 6,542
For SBRT I mean. Sclerosis is a biological process.Forget about doing a cone beam, I can’t even bill for 3D to treat a sclerotic bone met, so I’m going to go with no. I’m surprised we can even still ct sim them at this point.
D
deleted1180461
What? Everything is a biological process. After eating Taco Bell I have lots of biological processs.For SBRT I mean. Sclerosis is a biological process.
- Joined
- Sep 7, 2014
- Messages
- 3,566
- Reaction score
- 6,542
Totally. I don't really understand why the B in BGRT. that's what we do. Should be called UEEIIGRT. Unnecessarily expensive and entirely inconsequential IGRT.What? Everything is a biological process. After eating Taco Bell I have lots of biological processs.
- Joined
- Feb 11, 2005
- Messages
- 601
- Reaction score
- 483
Reflexion allows for the PET signal to be monitored in real time and for radiation to be directed at it. How that benefits the patient (vs Cyberknife or other real-time monitoring or adaptive planning systems that actually account for day to day changes) I don’t know.
D
deleted1180461
Theoretically you could get definitive doses to mobile tumors with limiting OARs eg, pancreas? The strategy now is basically to accept under dosing at the margins to ablate the center of the tumor. Ie, marginal miss because you have no choice. If the tech could wait until the tumor was a favorable location before beam on, then I could see a benefit. Bone Mets tend to be uh pretty easy to localize.Reflexion allows for the PET signal to be monitored in real time and for radiation to be directed at it. How that benefits the patient (vs Cyberknife or other real-time monitoring or adaptive planning systems that actually account for day to day changes) I don’t know.
- Joined
- Jul 14, 2020
- Messages
- 1,621
- Reaction score
- 4,726
Fabulous tool for basic research then. I have no idea what real time PET signal means in an actively irradiated target.Reflexion allows for the PET signal to be monitored in real time
Spatial resolution of PET typically quoted around 4-5 mm. Is this notably different on the reflexion? (All practicing radoncs will note the slice thickness they employ at CT sim and fused MRI when doing SBRT presently).
- Joined
- Sep 7, 2014
- Messages
- 3,566
- Reaction score
- 6,542
The mere fact that they tweeted about doing this to a bone met is in-line with something that they think will ultimately impress patients and annoy SDN/serve no purpose.
- Joined
- Jan 15, 2020
- Messages
- 45
- Reaction score
- 76
ELI5?What? Everything is a biological process. After eating Taco Bell I have lots of biological processs.
D
deleted1180461
You really want to know what 3 cheesy bean and rice burritos does to you? Good rad onc lunch btw. $4 meal.ELI5?
- Joined
- Jun 21, 2022
- Messages
- 1,350
- Reaction score
- 4,541
Theoretically you could get definitive doses to mobile tumors with limiting OARs eg, pancreas? The strategy now is basically to accept under dosing at the margins to ablate the center of the tumor. Ie, marginal miss because you have no choice.
What is the best imaging modality to look at a soft tissue interface between two organs? Not PET.
So, gating?If the tech could wait until the tumor was a favorable location before beam on, then I could see a benefit. Bone Mets tend to be uh pretty easy to localize.
I feel like a chump for trying to pretend this about clinical medicine. Im sitting here wondering what this is good far when the answer is right there on Jordan's spreadsheet.
Theoretically you could get definitive doses to mobile tumors with limiting OARs eg, pancreas? The strategy now is basically to accept under dosing at the margins to ablate the center of the tumor. Ie, marginal miss because you have no choice. If the tech could wait until the tumor was a favorable location before beam on, then I could see a benefit. Bone Mets tend to be uh pretty easy to localize.
I dont actually agree that this is the advantage of OTA for pancreas. This is pure hypothesis, but I think the cumulative CTV coverage is MUCH higher than if you just did your safe offline sim plan and delivered that with the PTV undercoverage/PRV uncertainty. When I would cover these cases, most would have substantial increases in coverage, like 50-->75%. This is obviously anecdotal.
It also kind of idiot proofs the RT planning and IGRT/delivery. Sometimes in my current practice I might be a little less aggressive on my CTV coverage because the patient is less stable or the set up might be more challenging.
They dont really have dose accumulation software yet that is ready for prime time, so we dont really know quantitatively.
Its also not like the primary method of failure is marginal local recurrence in these cases.
I was very hyped about the phase III adaptive trial for pancreas but was not very confident it would be a positive trial. I am not sure. I guess now it doesnt matter. COH has already declared the Viewray lifesaving and no one is going to run that trial.
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
One shot curative prostate RT.
That sounds so Zilli.
At least not calling it virtual prostatectomy. (Imagine how we’d describe virtually supervising virtual prostatectomies.)
- Joined
- Nov 2, 2019
- Messages
- 3,601
- Reaction score
- 14,885
Oh yeah.
Lemme tell you guys.
If there's one thing I love.
It's any "new" style of prostate cancer treatment.
With 18 months of follow-up data.
Totally worth the paper it's printed on.
- Joined
- Sep 20, 2004
- Messages
- 12,496
- Reaction score
- 13,040
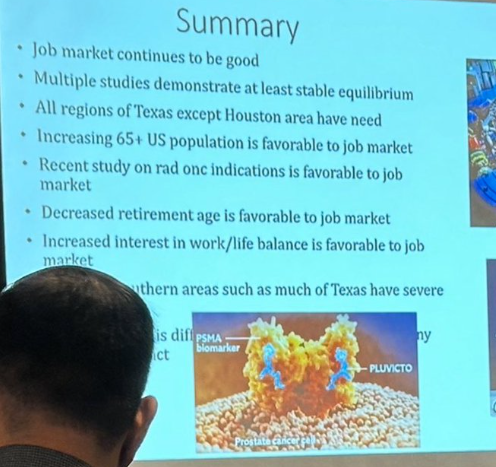
I know for certain several bullet points on that slide are demonstrably wrong
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
isn’t like Houston the most population dense area of TX. “All regions of TX except Houston area have a need for rad oncs.” So we need rad oncs… just not where there’s the most people. Try having that make good sense to a med student looking at rad onc vs say med onc, urology, etc.I know for certain several bullet points on that slide are demonstrably wrong
- Joined
- Sep 20, 2004
- Messages
- 12,496
- Reaction score
- 13,040
feel like I see pulm offering CT screening to pts a lot more in my neck of the woods than the PCPs do
"All regions of TX except Houston area have a need for rad oncs" is a very, very false statement.isn’t like Houston the most population dense area of TX. “All regions of TX except Houston area have a need for rad oncs.” So we need rad oncs… just not where there’s the most people. Try having that make good sense to a med student looking at rad onc vs say med onc, urology, etc.
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
Explain!"All regions of TX except Houston area have a need for rad oncs" is a very, very false statement.
- Joined
- Apr 28, 2005
- Messages
- 1,326
- Reaction score
- 3,776
Employed Rad Onc opportunities in Laredo and El Paso are available = all of Texas except the Houston area.Explain!
- Joined
- Sep 20, 2004
- Messages
- 12,496
- Reaction score
- 13,040
It's like they don't even try to pretend it's rain anymore. They just openly piss on residents these days"All regions of TX except Houston area have a need for rad oncs" is a very, very false statement.
Last edited:
I would but it would be an auto-doxx- I'll send you a pmExplain!
- Joined
- Jun 21, 2022
- Messages
- 1,350
- Reaction score
- 4,541
feel like I see pulm offering CT screening to pts a lot more in my neck of the woods than the PCPs do
This is just for HEDIS so it only matters for medicare and/or if your payer or employer track these measures and use them to make you do things. So this might make PCPs do it more.
It seems to me there has been a shift where culturally LCS is much more accepted than when I first started working on this at my job(s) 5 years ago. I know it is controversial but I think its a good thing for patients of lower SE status and states with heavy smoking.
Its also a slight good for Rad Onc. LCS programs consistently identify 2-4% of their cases as cancer and those patients seem to receive SBRT at least half the time, more in some systems.
- Joined
- Sep 20, 2004
- Messages
- 12,496
- Reaction score
- 13,040
Absolutely. Many of these pts with terrible lungs can't even get biopsies in some cases, just document growth, pet fdg avidity and beam on if pulm feels bx too risky and CT surgery doesn't want to wedgeThis is just for HEDIS so it only matters for medicare and/or if your payer or employer track these measures and use them to make you do things. So this might make PCPs do it more.
It seems to me there has been a shift where culturally LCS is much more accepted than when I first started working on this at my job(s) 5 years ago. I know it is controversial but I think its a good thing for patients of lower SE status and states with heavy smoking.
Its also a slight good for Rad Onc. LCS programs consistently identify 2-4% of their cases as cancer and those patients seem to receive SBRT at least half the time, more in some systems.
- Joined
- Dec 21, 2018
- Messages
- 237
- Reaction score
- 921
Lol
"Weather is great outside today, what climate change?"
"Weather is great outside today, what climate change?"
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
The rising incidence of stage one is “causing” the falling incidence of stage III. Also one new stage one lung patient consult per week adds one patient per day on beam, but one stage III consult per week would add 6 patients per day on beam. All of this is to say, it is not clear that significantly more lung cancer patients are seen per year per rad onc today than 20 years ago even with a dramatic uptake in LCS, and some data shows less lung patients per day per rad onc under beam. This math is very interesting.This is just for HEDIS so it only matters for medicare and/or if your payer or employer track these measures and use them to make you do things. So this might make PCPs do it more.
It seems to me there has been a shift where culturally LCS is much more accepted than when I first started working on this at my job(s) 5 years ago. I know it is controversial but I think its a good thing for patients of lower SE status and states with heavy smoking.
It’s also a slight good for Rad Onc. LCS programs consistently identify 2-4% of their cases as cancer and those patients seem to receive SBRT at least half the time, more in some systems.
D
deleted1180461
isn’t like Houston the most population dense area of TX. “All regions of TX except Houston area have a need for rad oncs.” So we need rad oncs… just not where there’s the most people. Try having that make good sense to a med student looking at rad onc vs say med onc, urology, etc.
It’s about as intellectually honest as pointing to a color map of national election results county by county and concluding a “red wave”
There isn’t competition for work in the Austin, Dallas, and San Antonio metros? I don’t believe that.
Oh people don’t want to move their families to the border towns? Big shocker there.
Places like Abilene are going to struggle to recruit because they are not going to pay any significant premium over what MDACC does. That’s their problem.
D
deleted1180461
As stage 3s or 1s?Just to throw out there - I’ve treated a few stage IIIs picked up on screening
I’ve seen a system that basically SBRTs anything remotely active on pet. Evaluating nodes and attempting biopsy? Nobody got time for that. Rad oncs eager to do it too. What was PPV of nodules picked up on the screening trials? Don’t ask questions…
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
Oh for sure. It happens. But this is the trend:Just to throw out there - I’ve treated a few stage IIIs picked up on screening
- Joined
- Dec 17, 2007
- Messages
- 3,783
- Reaction score
- 5,378
One major chance that I am seeing among physicians in Europe is part-time work.
I am not exactly sure, why this is not a thing in the US (or maybe it is)?
There are even residents nowadays that will work only something like 60% or 80% of the normal week. And no, they are not mums or dads with kids home, they are people with "hobbies". They choose a longer residence and less pay, in exchange for more free time. Needless to say, they keep this up after they've finished residency too.
Is this less common in the US, especially in the generation of physicians that have finished residency recently?
I am not exactly sure, why this is not a thing in the US (or maybe it is)?
There are even residents nowadays that will work only something like 60% or 80% of the normal week. And no, they are not mums or dads with kids home, they are people with "hobbies". They choose a longer residence and less pay, in exchange for more free time. Needless to say, they keep this up after they've finished residency too.
Is this less common in the US, especially in the generation of physicians that have finished residency recently?
No, we see this too, except I think we're coming from different starting points. Doctors in the US worked long hours, and a "busy" radonc could have 40-60 patients on treatment. There are still some that do, but it's much rarer/less desired by new grads these days, especially since the potential reward is much lower.One major chance that I am seeing among physicians in Europe is part-time work.
I am not exactly sure, why this is not a thing in the US (or maybe it is)?
There are even residents nowadays that will work only something like 60% or 80% of the normal week. And no, they are not mums or dads with kids home, they are people with "hobbies". They choose a longer residence and less pay, in exchange for more free time. Needless to say, they keep this up after they've finished residency too.
Is this less common in the US, especially in the generation of physicians that have finished residency recently?
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
Part time in America is still very sporadic. Mostly because of real and/or imagined supervision issues. As the real continues to become no longer real, and boogeyman stories lose their bite, part time will become much more common.One major chance that I am seeing among physicians in Europe is part-time work.
I am not exactly sure, why this is not a thing in the US (or maybe it is)?
There are even residents nowadays that will work only something like 60% or 80% of the normal week. And no, they are not mums or dads with kids home, they are people with "hobbies". They choose a longer residence and less pay, in exchange for more free time. Needless to say, they keep this up after they've finished residency too.
Is this less common in the US, especially in the generation of physicians that have finished residency recently?
D
deleted1180461
Part time in America is still very sporadic. Mostly because of real and/or imagined supervision issues. As the real continues to become no longer real, and boogeyman stories lose their bite, part time will become much more common.
Any rad onc signing up for a solo practice at a rural hospital that requires 5 days on site while linac is on is doing it wrong at this point.
- Joined
- Apr 3, 2019
- Messages
- 5,006
- Reaction score
- 11,486
I guess, but what if that’s the only job you can get and the bosses say “this is just how it is”?Any rad onc signing up for a solo practice at a rural hospital that requires 5 days on site while linac is on is doing it wrong at this point.
- Joined
- Aug 23, 2014
- Messages
- 3,353
- Reaction score
- 6,877
It is nice to see hellpits “lead”, prolific SOAP place wanting warm bodiesLol
View attachment 383178
View attachment 383180
"Weather is great outside today, what climate change?"

