- Joined
- Nov 17, 2019
- Messages
- 5
- Reaction score
- 28
- Points
- 321
- Resident [Any Field]
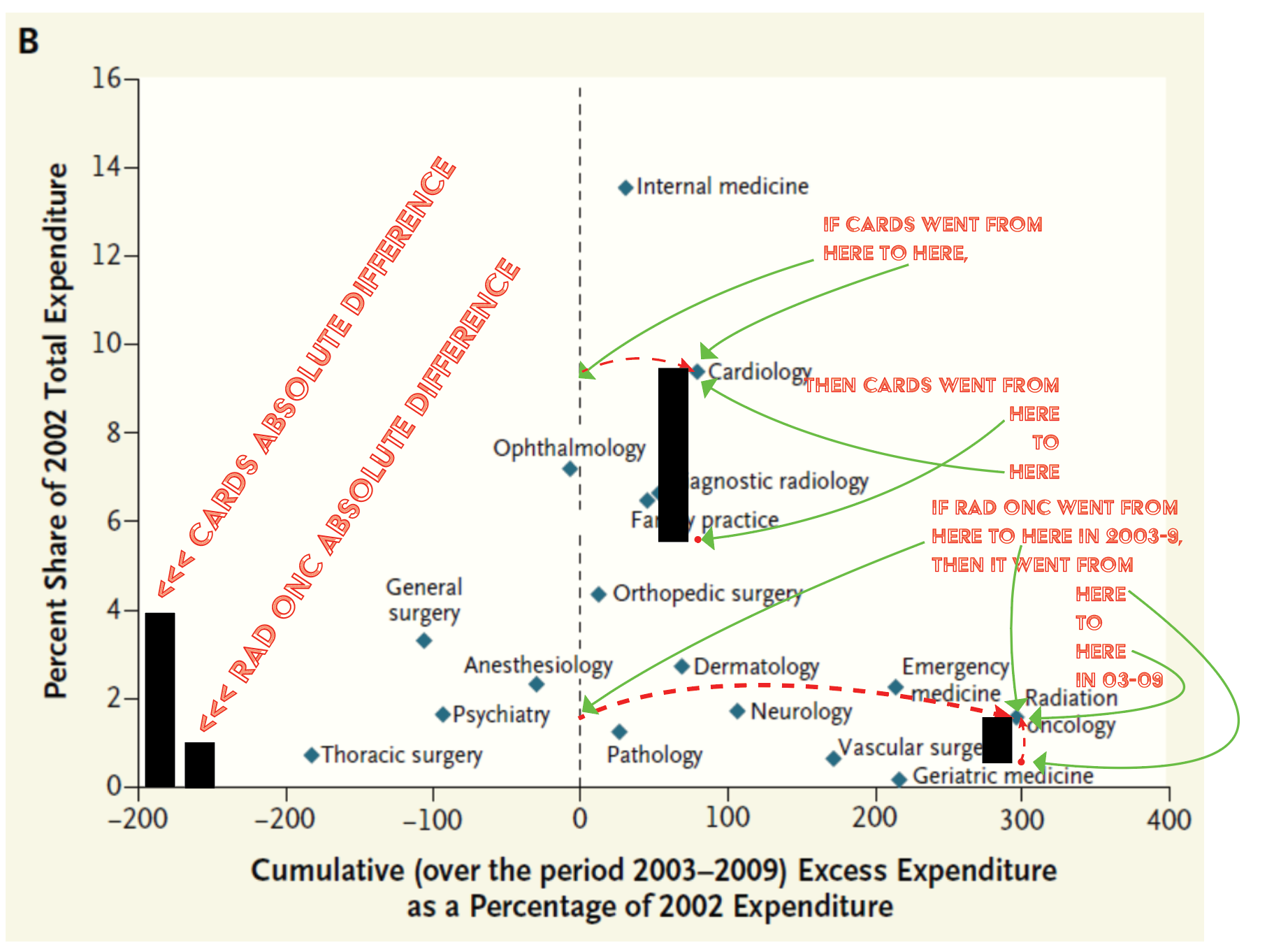
Exactly this. It is very depressing to be midway through residency, and to essentially be hearing from everyone ahead of you that you should have very little hope for your future career.All students: that ↑↑ this guy ↑↑ is having ANY job-finding pain is a huge indictment of rad onc, a big blinking red light saying STAY AWAYYYYY.
Like most current/recently graduated residents, I had >250 step 1/2, publications, and graduated at the top of my class. I worked my ass off to get here, and put in more time than most of my colleagues in other specialties. I felt like I matched into my dream specialty, but now I have to wonder if I’ll even have A job after all of this, much less a desirable one. Now, I feel like...how did I get here? I thought I was doing well in the grand scheme of things. Now, I can’t even feel proud about my accomplishments or hopeful about my future in this “dumpster fire” of a career field. Meanwhile, I’m seeing classmates starting their fellowships and attendingships, mostly exactly where they want to be geographically and career-wise.
I probably would have been a great candidate for rads or a top-tier IM program, and tbh I regret not choosing the IM>heme/onc path. Obviously, I read about the job market concerns before I applied, but I was also told by “mentors” that the situation wasn’t so desperate and it would turn around eventually as we’ve seen with other fields. I was told told to expect some geographic limitations, along the lines of “you might not end up in NYC or LA, but you‘ll be able to find something the state/region of preference”. I was told that this is still a great field with a great future, by the heads of programs and departments in this field, and why wouldn’t I have trusted them as a medical student? I’m sure many of you have had similar experiences. And this was still one of the most competitive fields to match, and why would “the best of the best” applicants still be applying if the doom and gloom were true?
Thankfully, seems like med students have absolutely wised up, and maybe it’s that the voice of the younger generation of rad oncs who have been yelling at the top of their lungs about these issues and are finally being acknowledged (seemingly by everyone EXCEPT leadership). I still think it is wholly unethical for our so called “mentors” and leaders still try to stoke any interest in this field for current med students, especially highly accomplished/desirable residency candidates.
I still love most aspects of working in radiation oncology, and in a perfect world, I don’t think any other field would have been a better fit for me. But the world is far from perfect rn, and enjoying the day-to-day work just isn’t worth the constant anxiety that myself and my coresidents have of a hopeless future in a seemingly irreparably broken field, before our careers as doctors have even really started.
Med students, PLEASE consider that this is what you would have to be dealing with 3 or 4 years down the line. It is NOT worth it.