Trying to give SBRT for an oligomet in the spine before the patient goes on to get carbo/Alimta/pembro. Med onc asking if there is a wash out period for the radiation. I'm thinking last fraction on a Friday, then start chemo on Monday should be enough time to avoid myelopathy. Radiobiologically, most DS-DNA repair from radiation happens in minutes to hours, so anything over 24 hours should be okay? Radbio instructors and PGY-5s, help me out!
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Radiation “wash out”?
- Thread starter w00tz
- Start date
- Joined
- May 10, 2009
- Messages
- 117
- Reaction score
- 287
Radiation myelopathy is something that happens a year or two down the line. Possible myelin damage can happen sooner (not myelopathy), but usually takes a few months at least. Should be fine to start chemo on Monday. Only thing to consider is a a short steroid taper to reduce the risk of edema/pain. It's something to consider with any spine SBRT case.
- Joined
- Oct 10, 2011
- Messages
- 8,624
- Reaction score
- 10,698
I usually just ask that full chemo (Something like carbo/alimta, not IO alone) be given after SBRT is over, not on the same day. I would not worry about 'radiation wash out'.
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
I wish we could peer down at the cellular level with cameras that had billion hertz frame rates and see what was happening. What I picture is that photons come in and interact mostly with the water, ionization happens to the water molecules, those free radicals (spurs, blobs, etc) "fizz" around, there are changes at the covalent bond level in the DNA molecule from this (which obviously cause covalent bond changes in the free radical instigators too). All of that is happening very rapidly. I think there's somewhere in Hall where it says this "chemistry dance" is over in 1/100,000th of a second after the last MU pulse comes in. Which naturally leads one to think, since the pulses happen every 1/5th to 1/40th of a second (ie 300 to 2400 MU/min dose rates in most machines), that radiation is "washing in" and "washing out" lots and lots of times just over one RT session. So I would have answered that radiation washes out in 1/100,000th of a second in terms of the immediate chemistry. The genetic changes however can last indefinitely... or be repaired rather quickly as you mention. When a genetic change from RT is repaired, is that "radiation washout"? To me the word "washout" conjures different imagery. We can think of some clinical examples e.g. "radiation recall" where those genetic changes from the RT are ever-present and ready to be "declared" by giving someone chemo. If viewed from this standpoint radiation never washes out (especially in late responding tissues); there's monkey data that the cord is still repairing RT genetic changes months after the RT (but not so much after a year... maybe). Hence it's safe to give the chemo 1/100,000th second after the RT, or it's not safe to ever give it. It's impossible to tell.wash out period for the radiation.
Last edited:
- Joined
- Oct 4, 2017
- Messages
- 5,016
- Reaction score
- 9,782
Second above. Only time I won’t give xrt on same day would be full dose taxane or gem. And in cases of melanoma- multiple beams with high energy if braf inhibitor to avoid skin toxicity
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
Now that SDN puts these "similar threads" links at the bottom of the page, I am sure you all see this one (and our beloved @Neuronix even commented on it):
I don't know what the case turned out to be, but the plaintiffs couldn't prevail if all us experts agree radiation "washes out" in 24 hours. (And this was a very low dose compared to SBRT.)
Massive pediatric radiation overdose
I don't know what the case turned out to be, but the plaintiffs couldn't prevail if all us experts agree radiation "washes out" in 24 hours. (And this was a very low dose compared to SBRT.)
- Joined
- Dec 2, 2011
- Messages
- 1,486
- Reaction score
- 3,009
Second above. Only time I won’t give xrt on same day would be full dose taxane or gem. And in cases of melanoma- multiple beams with high energy if braf inhibitor to avoid skin toxicity
I try to avoid pelvic RT with concurrent cyclophosphamide too.
There is no radiation wash out. The reason I have them hold off until the following day is purely logistical. We know how things go. Patient gets delayed coming or goes to med onc first and what do you know, they get the chemo and then come down for radiation. Overly cautious? Maybe.
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
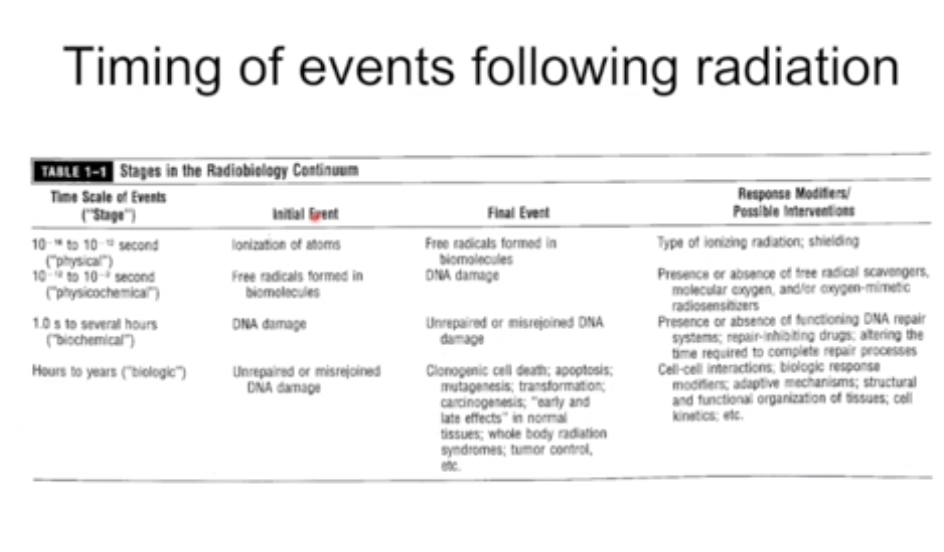
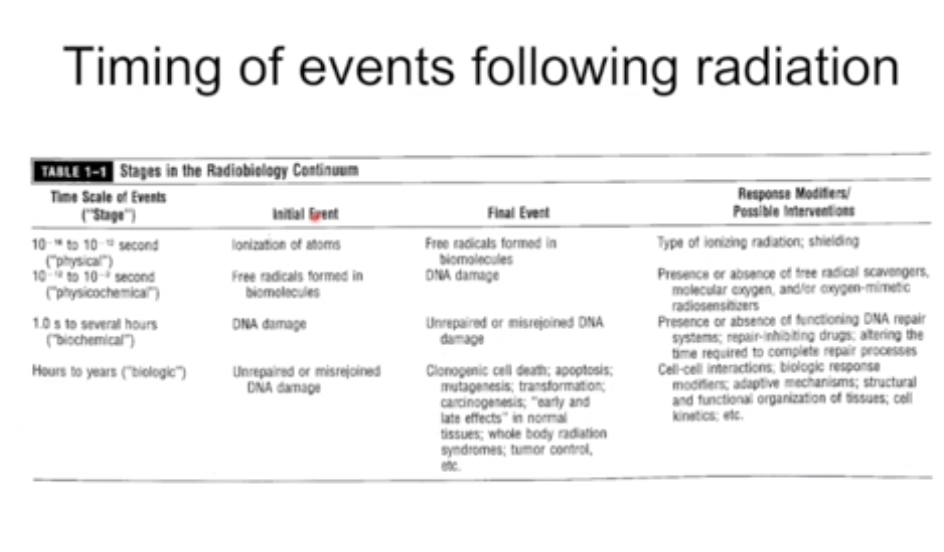
Here's what I was getting at; sorry it's difficult to read. This is from the recent ARRO-promulgated rad bio lecture series. The radiation washout happens in nanoseconds, or a century (in a centenarian).
There are like 17 trials looking at SBRT with immunotherapy for lung cancer and some do concurrent io. Food for thought.
I'm not worried as much about immunotherapy as I am with the cytotoxic agents. Had an attending repeatedly tell me about a case that haunted him. He was giving palliative spine radiation and the med onc gave concurrent taxane without telling him and the patient ended up in a wheelchair. No major structural spine issues.
- Joined
- Dec 2, 2011
- Messages
- 1,486
- Reaction score
- 3,009
I'm not worried as much about immunotherapy as I am with the cytotoxic agents. Had an attending repeatedly tell me about a case that haunted him. He was giving palliative spine radiation and the med onc gave concurrent taxane without telling him and the patient ended up in a wheelchair. No major structural spine issues.
I had a really bad complication on a day I passed a black cat on the way into work once too. In all seriousness, its probably unrelated. Think about how often we end up doing RT for cord compression (etc) right after people get full dose systemic therapy. If taxanes were that potent with RT we would use them even more than we do. The only drug class I do everything I can to avoid giving with RT are angiogenisis inhibitors. The risk of bowel perforation and fistulization is very real and well described. People can get pretty f@cked up if they are on high doses of methotrexate too. Pretty much everything else is along the lines of I know someone who had a friend who treated a guy and something bad happened (at least for severe toxicities, not just mucositis and such).
Last edited:
- Joined
- Dec 18, 2015
- Messages
- 3,216
- Reaction score
- 4,930
I'm not worried as much about immunotherapy as I am with the cytotoxic agents. Had an attending repeatedly tell me about a case that haunted him. He was giving palliative spine radiation and the med onc gave concurrent taxane without telling him and the patient ended up in a wheelchair. No major structural spine issues.
Welllll... that’s concurrent. Totally different animal. Another animal I’m not that familiar with is “acute radiation myelitis” except maybe at RT fraction doses over 8 to 10 Gy. I am familiar with patients with spine mets who get palliative RT and wind up in a wheelchair though at some time before they die. Henry Marsh said something to the effect “Every surgeon has a graveyard in his mind where he goes to pray from time to time.” But yes we all want to stay out of the graveyard.I'm not worried as much about immunotherapy as I am with the cytotoxic agents. Had an attending repeatedly tell me about a case that haunted him. He was giving palliative spine radiation and the med onc gave concurrent taxane without telling him and the patient ended up in a wheelchair. No major structural spine issues.
Similar threads
- Replies
- 9
- Views
- 1K
