- Joined
- Jul 16, 2003
- Messages
- 6,443
- Reaction score
- 4,789
- Points
- 6,481
- Attending Physician
Advertisement - Members don't see this ad
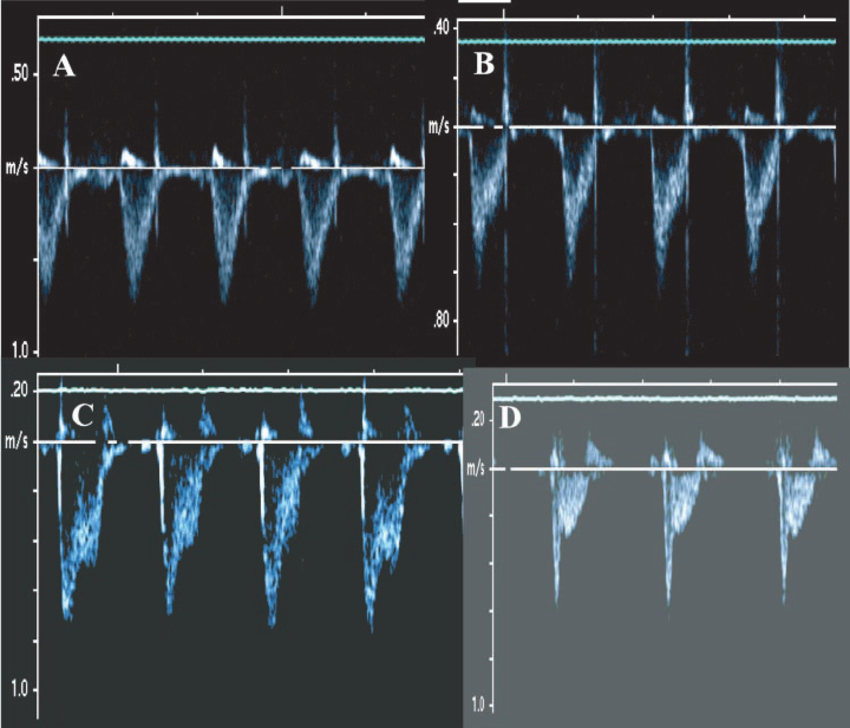
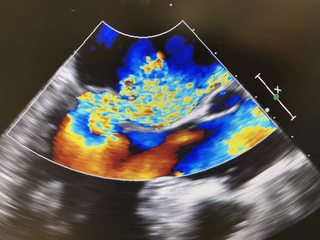
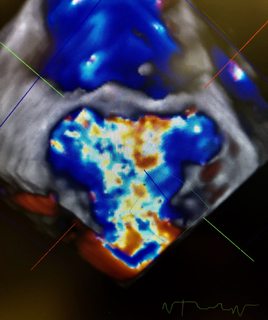
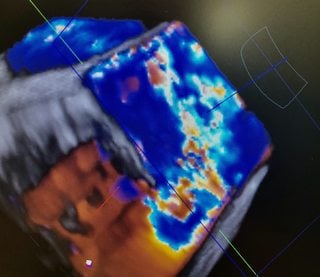
Question for you: when you MPR and crop the 3d color of one of these highly eccentric jets (i.e. the VC is essentially orthogonal from standard central MR), do you think you're able to get a frame where you you can trace an accurate vena contracta area?
You are taking your VC area measurements on the LV side of things, so I think the direction of the jet is a little less important although you want to apply planimetry to the VC en face.
J peterman summed it up quite nicely. If your frame rates are high enough on 2d MPR Pisa you can find it's narrowest point and take a VC area there. Admittedly, I don't do this on every case as it's a little more time consuming in Qlab. I think it's more helpful pre-op when you are trying to add up multiple jets to asses severity.