- Joined
- Jun 9, 2016
- Messages
- 1,253
- Reaction score
- 2,228
I don’t think I’m quite ready to call OB to admit yet.
Sorry for the snarkiness. I was feeling a little RustedFox 😉
I accept all snark 🙂 shed be going icu regardless
I don’t think I’m quite ready to call OB to admit yet.
Sorry for the snarkiness. I was feeling a little RustedFox 😉
C’mon son, you gotta give us a real BP. Nobody is getting a 150/130 BP and saying “okay, that sounds legit. No need to repeat.”
Would favor this, and it’s basically my ddx. Only thing I’d add that probably isn’t relevant is that eclampsia is also a post partum Dx (up to 6-12weeks depending on source) should be considered with end organ damage and that bp. Still needs labs and Icu, call to her ob, abx, would probably get cta ctv and discuss with neuro if time course and hard findings were convincing.
Would depend on diagnosis at my hospital. ICU if CVA treated with tPA, venous sinus thrombosis, TTP, septic or hemorrhagic shock. L&D under OB if routine postpartum preeclampsia, endometritis, sepsis without shock, or mild blood loss anemia with normalized vitals and hemorrhage control.
Let’s see more of the case and see where it takes us.
I believe alkaline phosphate naturally goes up during pregnancy and specifically third trimester. May just not have gone down yet. Also up in HELLP I believe, but don’t suspect in this case with normal LFTs.
Sounds like methamphetamine intoxication with subsequent withdrawal. Probably contributed to preeclampsia. Doubt eclampsia, but I suppose partial seizure possible.
PRES on the differential, but seems unlikely given degree of hypertension.
Initially had me thinking cerebellar stroke vs. venous sinus thrombosis high on the differential. Saw one similar case once. Meth could also precipitate. Too drowsy initially to stand up and check Romberg/gait? What was the tPA discussion? CVA seemed unlikely given exam? Unclear timeframe? Recent delivery? Might consider a rapid MRI given unclear and within the window for tPA.
tPA was in the discussion, and given she still was having vag bleeding/spotting it was a no-go.
Meth can cause people to act crazy. Her symptomology initially was dysarthria with odd eye movements and a non-focal motor extremity exam, which progressed to worsening obtundation, --> tube, and unable to move the left side with normal CT Head and CTA Brain.
I really thought she would have had a LVO given how her exam changed.
Did not try to walk her...she got worse in the ED.
I spoke to Mom on the phone after she had been there for about 1 hour, and it wasn't too much help. Mom admitted she did meth "a few times recently" but didn't think she did it recently. Earlier in the day she was complaining of diarrhea, then had dizziness.
I was a little frustrated with this case because she was getting worse and I really didn't know what was going on
and when I talked to the ICU they were all about "is this subclinical status epilepticus" and "we have to talk to Neurology now" and "I don't now how to treat pre-eclampsia" and I told them about the Mg infusion and he basically ignored me and said "just call OB". It was an ICU doc that nobody here really likes.
More shortly.
Need some HELLP interns?
(nice job of hiding the platelets, just like my lab always does with ANY abnormality)
~ 700.
Dysarthria, gaze palsy, hemiparesis, unconsciousness points to a medial brain stem syndrome. Would get MRI as first priority. Infective encephalitis also possible so would treat that.
Venous thrombosis unlikely with that degree of coma but no CT findings. It’s not hypertensive PRES if the BP is now normal but getting worse. I would actually consider driving the blood pressure back up at this point and seeing if she improves.
Could also be postpartum cerebral vasoconstriction made worse by meth. MRI may find vasoconstricted vessels but not necessarily
This is outside of my area of expertise, but the little bit of PRES I've seen improved over a course of days. She seemed like she was already teetering on the edge, I'm not sure I'd rule out PRES based on continued deterioration over the course of an hour or so after BP normalization. I'm open to education though. Infectious or autoimmune encephalitis is a good thought and another that came to mind. I'm assuming she got AED loaded and shipped to MRI/V after tubed. Interested to see what it showed
posterior circulation stroke?
After being told that CTA Brain was OK, and I start transfusing and calling people like the ICU and OB.
I get a call 20 minutes later from the radiologist.
CTA Neck shows a narrowing of the R vertebral artery around C4. Could be thrombus / dissection.
I load her with aspirin 325 PR while transfusing pRBCs. I order a bunch of MRIs
I make more calls....and at the end of my shift the signout is "we are getting a STAT EEG in the ED, if negative pt is admitted here, if + then she needs to be transferred." That's the way it works at my shop. It sucks.
The next day I log into the EMR to see what happened.
View attachment 312338 View attachment 312339 View attachment 312340
View attachment 312341
MRV negative.
she self-extubated in the night and left AMA several hours later. Unable to walk well, she asked to be wheelchaired out to the car where her family member was waiting.
Not the most difficult case, as most Neurology emergencies have few proven ER interventions to make a difference. But nonetheless interesting and upsetting as she was in her 20s and now has a baby to take care of.
I make more calls....and at the end of my shift the signout is "we are getting a STAT EEG in the ED, if negative pt is admitted here, if + then she needs to be transferred." That's the way it works at my shop. It sucks.
she self-extubated in the night and left AMA several hours later. Unable to walk well, she asked to be wheelchaired out to the car where her family member was waiting.
What's the break point in admission VS transfer based on? Lack of neurotele?
This is true everywhere I have worked, continuous EEG usually can only be done in a true neuro-ICU, which is only at comprehensive stroke centers.
Yes...R vertebral artery dissection that was showering thrombus through the R PCA and even into the circle of willis. Hit parts of her brainstem as well. She had big bilateral stroke R > L.
While I believe that...I think the indications for continuous EEG are narrower than our ICU docs suggest. It's all for legal reasons. They openly admit that.
For instance, people with cardiac arrest, ROSC and need for TTM have something like a 25% chance of going into subclinical status epilepticus if I recall. We never transfer these patients. Why? $$$$
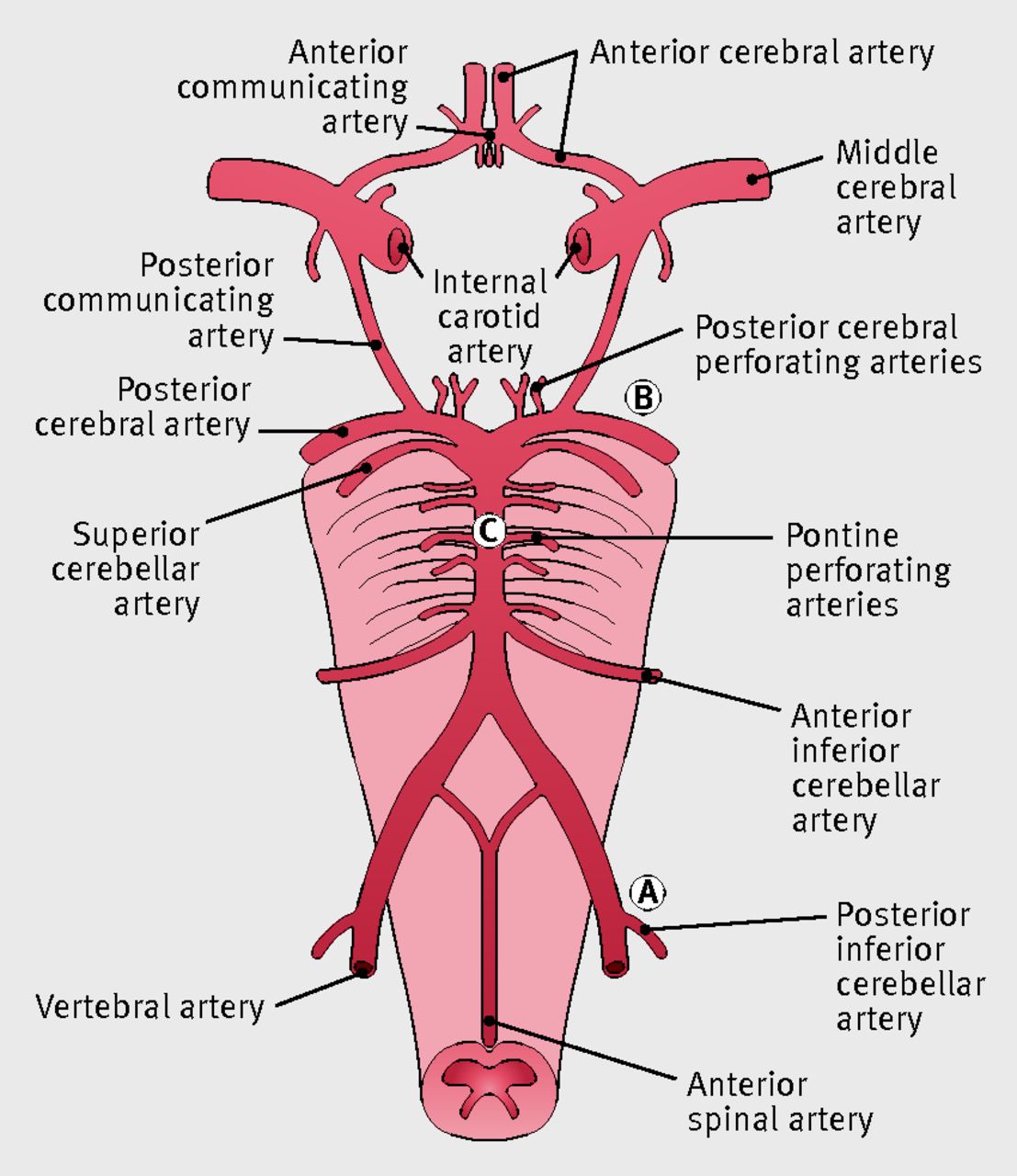
Odd that thromboemboli from the vert could reach anterior brain (maybe my neurovascular anatomy isn't great), but that explains why she had the left extremity weakness in addition to the nystagmus and ataxia.
I agree, I'm not sure what kind of intervention patient could have had. Did neuro re-consider tPA after the MRIs? Did they feel there was an unclear onset or the vaginal bleeding related to delivery felt to be a contraindication?
Seems the areas of ischemia are in areas of small vessel vasculature too small to go after with a catheter (again my neurovascular anatomy knowledge is not great), at least anticoagulation to try and stabilize any further thromboemboli from the dissection would be helpful. It seems this patient is probably not gonna be real consistent with the antiplatelet therapy I'm sure they discharged her on.
I'm guessing as far as ultimate etiology, pregnancy-delivery induced softening of connective tissue in a person with unknown susceptibility (undiagnosed perhaps untypable connective tissue disorder) precipitating dissection (pregnancy/delivery known risk factor for large and medium vessel dissection).
That's a good point, I have heard cited that NCSE is VERY under-diagnosed in ICU patients.
But I think the indication to monitor EEG in a patient with known uncontrolled seizure activity is a little stronger than in a patient who may hypothetically go into NCSE.
I've always kind of gone with the quote from the neuro-intensevist Thomas Bleck (and I'm parapharsing here) "Managing status epilepticus in a sedated patient without continuous EEG is like trying to run ACLS on a coding patient with your finger on the pulse but no continuous cardiac monitor."
That being said, I've had a few cases where I tubed a patient for status epilepticus, but it's during business hours (say 11am on a Wednesday) and the neurologist and EEG tech are actually available, stat evaluate the patient, do the EEG and determine the seizure is aborted. Usually at that point they feel comfortable recommending ICU admission rather than transfer and the intensevists are ok with that.
Management of status epilepticus. Our ICU docs believe that one must be on continuous EEG. Our Neurologists say that isn't necessarily true. Of course I believe our Neuro docs. Sometimes our Neurologist say no continuous EEG is needed and even the ICU docs wins out because they will refuse to consult on the case. Idiotic.

Out of curiosity, who said the CTA was clean? A vert dissection that big on MRA would be visible on CTA.After being told that CTA Brain was OK, and I start transfusing and calling people like the ICU and OB.
I get a call 20 minutes later from the radiologist.
View attachment 312341
Out of curiosity, who said the CTA was clean? A vert dissection that big on MRA would be visible on CTA.
Had an interesting one recently...
Now that's a case. Reinforces my usual practice of ignoring 'diarrhea' on ROS. I find that so many people endorse this symptom w/o really having it.
Now that's a case. Reinforces my usual practice of ignoring 'diarrhea' on ROS. I find that so many people endorse this symptom w/o really having it.
Sorry for the delayed reply, but a few points I keep thinking about.
Good for you in localizing the lesion. I spent a lot of time during medical school memorizing all of the various stroke patterns and even some time in residency revisiting as I felt you needed to know where the clot was at in order to decide if you should give/offer tPA. Since then I’ve seen a lot of thromboembolic strokes with unusual patterns that didn’t really fit a defined distribution on exam and ended up with evidence of shower phenomena on MRI.
During “stroke activations” I no longer spend mental power really trying to accurately localize the lesion. I instead spend my time on several factors:
1) Accurately trying to find out time of symptom onset. EMS, patients and family are often wrong. I try to get the most definitive answer from the patient, but also involve all sources to help elucidate.
2) Determine in general if pattern of symptoms/deficits most likely indicates a possible stroke. Bilateral leg weakness limited by back pain makes not seem likely. Altered with fever and dysarthria per the SNF staff seems unlikely. Hemiparesis with an odd CN exam seems more likely. Headache with diffuse extremity tingling seems unlikely. Left arm weakness with facial palsy seems more likely. Etc.
3) Complete NIHSS.
4) Fully run through tPA contraindications.
5) Consent patient/family making sure everyone is on board. This is one of the highest risk medications we give or don’t give. If there is a bad outcome I don’t want people pointing fingers.
Those 5 points take a lot of mental effort and time within a short time period. I think cognitive offload in high intensity situations is valuable. I haven’t found definitively localizing the lesion to be a good use of my brain power clinically any more. How do others feel?
Unless also with methamphetamine withdrawal post intoxication. These people snooze hard. Doesn’t mean they also couldn’t have a CTV.
In my prior experience as a resident in the ICU, MRI appearing PRES seemed to take days to resolve the encephalopathy despite a normalized BP with treatment.
How? By discontinuing Mg infusion in a preeclamptic patient and instead starting Levophed? I would strongly caution against driving the pressure up. You’ll hang yourself out to dry majority of the time by not treating preeclampsia appropriately if there is a bad outcome. I’m totally supportive of pushing the boundaries in critically ill patients if worsening, but I’m not sure this is the right case.
Sorry for the delayed reply, but a few points I keep thinking about.
Good for you in localizing the lesion. I spent a lot of time during medical school memorizing all of the various stroke patterns and even some time in residency revisiting as I felt you needed to know where the clot was at in order to decide if you should give/offer tPA. Since then I’ve seen a lot of thromboembolic strokes with unusual patterns that didn’t really fit a defined distribution on exam and ended up with evidence of shower phenomena on MRI.
During “stroke activations” I no longer spend mental power really trying to accurately localize the lesion. I instead spend my time on several factors:
1) Accurately trying to find out time of symptom onset. EMS, patients and family are often wrong. I try to get the most definitive answer from the patient, but also involve all sources to help elucidate.
2) Determine in general if pattern of symptoms/deficits most likely indicates a possible stroke. Bilateral leg weakness limited by back pain makes not seem likely. Altered with fever and dysarthria per the SNF staff seems unlikely. Hemiparesis with an odd CN exam seems more likely. Headache with diffuse extremity tingling seems unlikely. Left arm weakness with facial palsy seems more likely. Etc.
3) Complete NIHSS.
4) Fully run through tPA contraindications.
5) Consent patient/family making sure everyone is on board. This is one of the highest risk medications we give or don’t give. If there is a bad outcome I don’t want people pointing fingers.
Those 5 points take a lot of mental effort and time within a short time period. I think cognitive offload in high intensity situations is valuable. I haven’t found definitively localizing the lesion to be a good use of my brain power clinically any more. How do others feel?
Had a really weird case today... healthy young guy with left flank pain, LLQ abdominal pain, and a cold right foot. Dopplerable pop but no DP/PT. CTA A/P with runoffs showed left renal infarct and multiple emboli in both legs with total occlusion of the right distal popliteal. Also on CT? LV thrombus... COVID+.
What a wicked disease to say the least...
I think ativan can be appropriate in certain situations involving BIPAP. Yours was 100% NOT one of them. It's like sure, let's kill off whatever respiratory drive the patient has left with ativan...
Agreed.@thegenius Sometimes it calms them down enough to keep the mask on... but it depresses their respiratory drive as well. It's a difficult decision unfortunately. The only thing our nurses seem to ask more about is a blood pressure above 140. Sometimes I treat the nurse and not the patient -- just so they'll stop calling or posting comments in the trackboard.
There are other options to ativan for the severely anxious respiratory patient that is refusing to keep their bipap mask on despite the necessity. Especially when I am working my rural ER shifts, and I only have 2 nurses and 10 patients, I can't keep that nurse tied up trying to hold that patient down until the bipap starts working. Just give them a dose of haldol. It works well, and has minimal if any respiratory depression.Yesterday I had this extremely sick (albeit run-of-the-mill) flash pulmonary edema in a woman with an EF 25%. She was taking off her NIPPV saying "I can't breathe". She was per-intubation. I basically asked RT to stand next to her indefinitely and keep that mask on her while it, and the nitro gtt, took effect.
I had a nurse ask me "doc can we give her some ativan to calm her down?" I calmly said no. About 5 minutes later a different nurse asked the same question, and this time I snapped a little as I sternly said "It's NOT a treatment for flash pulmonary edema. BiPap and nitrates are the two best things to give her right now."
What is it with the desire to give every single person in respiratory distress some ativan? I get so sick of that reflex sometimes.
Eh, this is a rhetorical question or comment than anything else.
There are other options to ativan for the severely anxious respiratory patient that is refusing to keep their bipap mask on despite the necessity. Especially when I am working my rural ER shifts, and I only have 2 nurses and 10 patients, I can't keep that nurse tied up trying to hold that patient down until the bipap starts working. Just give them a dose of haldol. It works well, and has minimal if any respiratory depression.
That’s some nonsense. Has your medical director not addressed that with the nursing admin?Haldol requires a 1:1 nursing assessment at my shop. Nurses hate me for using Haldol.
That’s some nonsense. Has your medical director not addressed that with the nursing admin?
Depends on the department and having reasonable nursing admin. Our medical director has gotten several ridiculous, out dated nursing policies changed. Sounds like you got either crap medical directors or terrible nursing admin, or a little of both.How much power and control do you think the medical director actually has over anything that happens in the department? And on who's side do you think most of them are?
Depends on the department and having reasonable nursing admin. Our medical director has gotten several ridiculous, out dated nursing policies changed. Sounds like you got either crap medical directors or terrible nursing admin, or a little of both.
