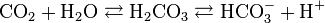
So, I am reading up on acid-base disturbances, which have always given me a bit of trouble. I think I am understanding them a lot better now, but am still confused about how the different lung diseases in particular cause either resp. acidosis or alkalosis. Different resources say different things and the sources I've taken a look at don't really do a good job of explainingthe reason why a particular disease causes acidosis or alkalosis.
Take for example, restrictive and obstructive lung diseases. I can understand that with an obstructive lung disease you have trouble getting air out of the lungs, so less CO2 is removed --> respiratory acidosis.
But what about restrictive lung disease? Different books say different things - some say that they cause resp. acidosis, while others say they cause resp. alkalosis. Nobody seems to give a good explanation either way. I think I can reason out that restrictive lung disease, esp. interstitial lung disease, --> imparied diffusion of CO2 out of the lungs --> resp. acidosis).
What about pulmonary edema and pneumonia? Some sources say resp acidosis and some say resp alkalosis?
Finally, one of the major causes I've seen for resp. alkalosis is hypoxemia (due to stimulation of peripheral chemoreceptors). However, it seems that most pulmonary causes of hypercapnia would also cause hypoxemia. So why wouldn't all pulmonary causes of hypercapnia cause a respiratory alkalosis?
Finally, I've noticed that severe anemia is listed as a cause of respiratory alkalosis, but can't find the mechanism for this. Since anemia only decreases O2 content and doesn't affect the PaO2, I'm guessing it has nothing to do with peripheral chemoreceptor stimulation...
Take for example, restrictive and obstructive lung diseases. I can understand that with an obstructive lung disease you have trouble getting air out of the lungs, so less CO2 is removed --> respiratory acidosis.
But what about restrictive lung disease? Different books say different things - some say that they cause resp. acidosis, while others say they cause resp. alkalosis. Nobody seems to give a good explanation either way. I think I can reason out that restrictive lung disease, esp. interstitial lung disease, --> imparied diffusion of CO2 out of the lungs --> resp. acidosis).
What about pulmonary edema and pneumonia? Some sources say resp acidosis and some say resp alkalosis?
Finally, one of the major causes I've seen for resp. alkalosis is hypoxemia (due to stimulation of peripheral chemoreceptors). However, it seems that most pulmonary causes of hypercapnia would also cause hypoxemia. So why wouldn't all pulmonary causes of hypercapnia cause a respiratory alkalosis?
Finally, I've noticed that severe anemia is listed as a cause of respiratory alkalosis, but can't find the mechanism for this. Since anemia only decreases O2 content and doesn't affect the PaO2, I'm guessing it has nothing to do with peripheral chemoreceptor stimulation...