- Joined
- Sep 17, 2016
- Messages
- 778
- Reaction score
- 1,251
- Points
- 5,276
- Age
- 38
- Attending Physician
As I learned from a CRNA recently, just give propofol 50mg to a low EF 30s 80 year old patient. They’ll be fine.
I'd recommend everyone be comfy ish with these drugs as boluses. You can keep a big mac alive with themCould you give us some numbers (mg) for the boluses? Honestly, I've only used norepi as an infusion :/
I'd recommend everyone be comfy ish with these drugs as boluses. You can keep a big mac alive with them
Norepi put 4mg vial in 100ml bag so 40mcg per mil, take 1 mil and dilute into 10ml syringe so 4mcg per ml. 1 or 2 ml then push at a time
Epi put 1mg in 100ml bag that's 10mcg per mil. Push 1 to 3 mls at a time in a crashing patient. No more crash
Vaso is 20unit in a vial of 20ml. Push half a mil at time. Approx equipotent to 10mcg of epi in my limited experience
Milrinone push half an mg or 1mg at a time. Comes in 1mg per ml vial. With a vaso chaser of half to 1 unit. Works great too
As for the crna pushing 50mg propofol lol. A resident did that last year when I allowed too much trust. Never again. Propofol is a lethal weapon around these people
I feel like small epi boluses work great. No matter the situation. Just a dab will do ya!I can think of no situation where pushing a milrinone 1/8 to 1/4 loading dose (~6-12 mcg/kg) is warranted.
Even in a situation like a protamine reaction with severe pulm HTN and acute right ventricular failure, you're likely going to cause the pt to arrest if you push some milrinone. Vasopressin chaser or not, milrinone boluses can still cause profound hypotension which (to say the least) is not ideal in a scenario where you want to maintain aortic diastolic blood pressure so an acutely overpressurized RV can maintain luxury systolic and diastolic perfusion.
I can think of no situation where pushing a milrinone 1/8 to 1/4 loading dose (~6-12 mcg/kg) is warranted.
Even in a situation like a protamine reaction with severe pulm HTN and acute right ventricular failure, you're likely going to cause the pt to arrest if you push some milrinone. Vasopressin chaser or not, milrinone boluses can still cause profound hypotension which (to say the least) is not ideal in a scenario where you want to maintain aortic diastolic blood pressure so an acutely overpressurized RV can maintain luxury systolic and diastolic perfusion.
only pushed milrinone 1mg at a time once... ended up giving like 5mg total. and it worked well. n=1...
What was the scenario
Ok it's a high dose but I've seen it quite a bit and I got it from our chief cardiac anesthesia prof. He would use it on difficult weans from cpb.I can think of no situation where pushing a milrinone 1/8 to 1/4 loading dose (~6-12 mcg/kg) is warranted.
Even in a situation like a protamine reaction with severe pulm HTN and acute right ventricular failure, you're likely going to cause the pt to arrest if you push some milrinone. Vasopressin chaser or not, milrinone boluses can still cause profound hypotension which (to say the least) is not ideal in a scenario where you want to maintain aortic diastolic blood pressure so an acutely overpressurized RV can maintain luxury systolic and diastolic perfusion.
Being comfy with pushes is in our wheelhouse, for sure. I agree with the can’t imagine case for milrinone bonus camp - sounds like a great way to bottom out the pressure. If you’re really struggling and need an ionotrope for the RV (think acute PE) - think EPI.
what about RV due to pHTN? milrinone isn't going to get rid of the PE and fix the pulmonary issue, but it helps with pHTN
what about RV due to pHTN? milrinone isn't going to get rid of the PE and fix the pulmonary issue, but it helps with pHTN
This is so basic knowledge that, if anyone didn't know this BEFORE reading your post, they should not even consider playing with advanced inotropes and pressors.Mi”rinone only causes major hypotension if you’re not expecting it to work (make the heart snap more).
This is something that I believe many don’t understand. If you give milrinine to a heart with some contractility reserve, the increased stroke vigor balances the vasodilation. If you’re looking at a dead heart that probably won’t snap any harder (large areas of ischemic myocardium), then of course giving milrinone will mostly cause vasodilation with no CO to balance it.
Don’t give milrinone unless you think the myocardium that isn’t snapping is likely to snap harder. Or if something else will prevent an increase in cardiac output like AS or pulmonary artery hypertension/ obstruction
There is so much "pulmonary HTN" due to left heart disease (e.g. diastolic dysfunction) that's misdiagnosed, even by pulmonary docs. The RV may be "failing" because the LV is failing (more frequently than one would think). It's the so-called biventricular HF reflex (from the Manual for Pulmonary and Critical Care Medicine by Landsberg):Start an infusion instead if you feel like it’s warranted, and use vasopressin for hypotension rather than phenylephrine. But it’s so easy to overreact to “pulmonary HTN” as a number.
This is so basic knowledge that, if anyone didn't know this BEFORE reading your post, they should not even consider playing with advanced inotropes and pressors.
I am sticking to what I said before and you quoted.Lots of people don't understand why some people get very hypotensive with milrinone and others don't.
The right heart was one of the most interesting things I learned about in residency. I’m still confused by it and the diagnosis and management of RV failure and PA pressures. It’s not so straight forward IMO. Or maybe I’m just dumb...
I disagree. Paralyze, tube, keep them light.If General needed. Lma is preferred over geta as long as airway and other conditions are reasonable.
I disagree. Paralyze, tube, keep them light.
First, i would like to thank you for providing sources. You've already done a lot to engage me in this nerdy conversation and i appreciate it.Hi!
Without knowing which point you take umbrage with it's hard to target some citations to interest you and engage in a discussion, but here are a few, including various primary sources and meta-analyses.
Benzodiazepine use and postoperative delirium:
POSTOPERATIVE DELIRIUM - PMC
Delirium is an unfortunately common complication seen during the postoperative course. Because of its significant association with physical and cognitive morbidity, clinicians should be aware of evidence-based practices relating to the diagnosis, ...www.ncbi.nlm.nih.gov
Preoperative medication use and postoperative delirium: a systematic review - PMC
Medications are frequently reported as both predisposing factors and inducers of delirium. This review evaluated the available evidence and determined the magnitude of risk of postoperative delirium associated with preoperative medication use. A ...www.ncbi.nlm.nih.gov
Clinical risk factors associated with postoperative delirium and evaluation of delirium management and assessment team in lung and esophageal cancer patients - Journal of Pharmaceutical Health Care and Sciences
Background Delirium is an acute change in cognition and concentration that complicates the postoperative course. Patients who suffer delirium after surgery have an increased risk of persistent cognitive impairment, functional decline, and death. Postoperative delirium is also associated with an...jphcs.biomedcentral.com

Emergence delirium in adults in the post-anaesthesia care unit - PubMed
Preoperative benzodiazepines, breast and abdominal surgery and surgery of long duration are risk factors for emergence delirium.www.ncbi.nlm.nih.gov

Risk factors for inadequate emergence after anesthesia: emergence delirium and hypoactive emergence - PubMed
Inadequate emergence after anesthesia is a frequent complication. Preventable risk factors for emergence delirium were induction of anesthesia with etomidate, premedication with benzodiazepines and higher postoperative pain scores. Hypoactive emergence was less frequent than emergence delirium...www.ncbi.nlm.nih.gov
Postoperative delirium and perioperative mortality:
POSTOPERATIVE DELIRIUM (yes, a repeat!)
Postoperative Delirium: Acute Change with Long-Term Implications - PMC
Delirium is an acute change in cognition and attention, which may include alterations in consciousness and disorganized thinking. While delirium may affect any age group, it is most common in older patients, especially those with preexisting ...www.ncbi.nlm.nih.gov

Incidence of Postoperative Delirium and Its Impact on Outcomes After Transcatheter Aortic Valve Implantation - PubMed
There are limited data on the occurrence of postoperative delirium after transcatheter aortic valve implantation (TAVI). We sought to investigate the incidence of delirium after TAVI and its impact on clinical outcomes. A total of 148 consecutive patients who underwent TAVI were enrolled. Of...www.ncbi.nlm.nih.gov
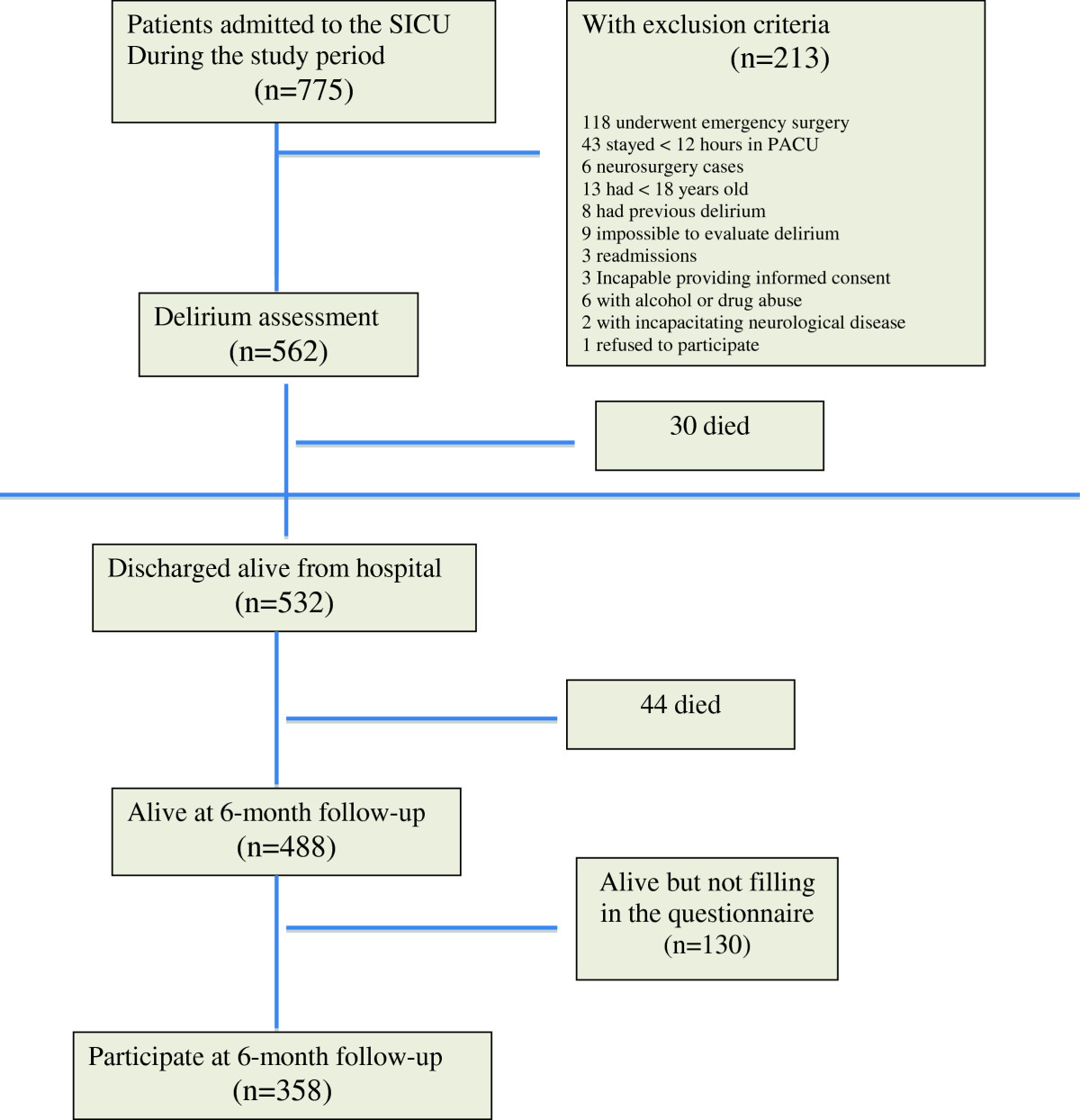
Outcome and quality of life in patients with postoperative delirium during an ICU stay following major surgery - Critical Care
Introduction Delirium is an acute disturbance of consciousness and cognition that has been shown to be associated with poor outcomes, including increased mortality. We aimed to evaluate outcome after postoperative delirium in a cohort of surgical intensive care unit (SICU) patients. Methods This...ccforum.biomedcentral.com
Anesthesiology
anesthesiology.pubs.asahq.org
Before getting into the weeds with this stuff, I'd love to understand what your particular quibble is in that quote so we can chat about it. I am not saying this is you, but if I hear "I've never heard of any randomized, double-blinded, placebo controlled trial that shows 2-5 mg of midaz pre-op causes delirium!!" (typically stated while pushing it in a completely chill, non-anxious 85 year old getting an arterial line), one more time, I am going to scream.
This is not a question of induction stability. In these patients who are often elderly and often develop an AKI secondary to hypoperfusion during their pump run, midazolam may not be the best choice. Benzodiazepines in general are implicated in postoperative delirium (and long term postoperative decline), especially in elderly folks [weak evidence if any at all with midazolam. It makes as much sense as giving 1mg of esmolol to a pt on chornic metoprolol is going to improve their survival 1 year later.]. Postoperative delirium is associated with increased mortality [very true I totally agree].
Your induction will be more stable. The patient's postoperative course may not be. This includes LVADs.
Sometimes I see CRNAs running 0.5 MAC gas and I get worried about awareness.
If there’s no narcotics or benzos on board, what MAC do you worry about awareness?Don't be
If there’s no narcotics or benzos on board, what MAC do you worry about awareness?
Where does this number come from? If it’s anecdotal experience it means nothing to me, awareness is too rare and anesthesiologists notoriously never follow up long enough after surgery to reliably catch awareness.Depends on the patient and surgical stimuli. Hugely. About 0.8% Sevo (0.4 MAC) is my number, too.
On the other hand, I tend to run a balanced anesthetic, and I give opiates, decadron, lidocaine etc. so the real "MAC" is higher.
Is anyone giving midaz to hypotensive pts intraop so they can reduce the amount of volatile? Sometimes I see CRNAs running 0.5 MAC gas and I get worried about awareness. I’d rather run higher gas with pressors but curious if anyone is giving midaz instead
I feel like small epi boluses work great. No matter the situation. Just a dab will do ya!
Where does this number come from? If it’s anecdotal experience it means nothing to me, awareness is too rare and anesthesiologists notoriously never follow up long enough after surgery to reliably catch awareness.
My number is typically 0.7 age adjusted MAC of all volatile.
I can think of no situation where pushing a milrinone 1/8 to 1/4 loading dose (~6-12 mcg/kg) is warranted.
Where does this number come from
You're coming off pump and the RV protection was questionable and the pt has Pulm HTN. you need to load your milirinone and you either give it to the perfusionist to give on pump or you push 5mg (or 1/2 vial of this yourself). Done it 3 or 4 times in residency.
Disagree. Awareness is rare enough but if you do have a case of it and you're at 0.5 you're screwed royallyDon't be
If RV protection is questionable and the pt has pHTN then you instruct the perfusionist and surgeon that we're not going to be coming off pump at the usual pace. Once the cross clamp is off and everyone is ready, let the heart fill a bit and if things look terrible then start a whiff of epi to get things snapping and load your milrinone over 5 minutes while you allow the heart rest on half- or quarter-flow CPB. You're not doing anyone any favors by rushing the process if you're expecting a difficult wean.
0.4 mac sevo is very different when there are other agents on board like fentanyl. if only PURELY volatile, I usually go ~0.7 mac for reliable amnesia
totally agree with not rushing off pump.
But what would be the advantage of slowly adding milrinone vs just pushing if the pt is on pump anyways. perfusionist is just sitting right there, cannulas are in? the patient needs a milirinone load if you want to start milirinone. youre prolonging the pump run by waiting for your .375 mcg/kg/min to take effect.
If you really think giving milirinone over 5 mins is that different than pushing it. I think that i would disagree.
how long since your last bolus do you consider fentanyl still "on board"? let's say you gave fentanyl 100mcg bolus 1 hour ago in a 64M 170cm 75kg male with HTN and DM2. do you still consider it "on board"? if 1 hour is no longer on board how long do you consider it "on board"?
Thats a very interesting questions, and I don't think it has a single "correct" answer. As with any bolused drug, you get a peak effect (usually overshoots your desired site effect concentration) and then a slow decreasing plasma (and site effect) concentration. Both depend on previous doses and clearance of the drug (which in turn depends on a lot of different factors). We can only relay on changes over time of very indirect measurements such as a BP, HR or maybe BIS?
Indeed MAC is always changing if you are using opioids in boluses doses, even if your etGAS % is stable over time. Some people will give standard boluses of narcotic every 1–2 hrs of X mg/kg or some people will wait for changes in vital sign trends.
how long since your last bolus do you consider fentanyl still "on board"? let's say you gave fentanyl 100mcg bolus 1 hour ago in a 64M 170cm 75kg male with HTN and DM2. do you still consider it "on board"? if 1 hour is no longer on board how long do you consider it "on board"?
As far as I know, vital sign changes have never been validated as a marker of depth of anesthesia. But that doesnt really change the fact that me and literally every other anesthesiologist in the world uses them for that purpose.
So true lol
But my point was not using it as a marker of depth of anesthesia but of narcotic effect in blunting the sympathetic response to surgical stimuli (regarding the comment of until when we consider that a dose of narcotic is still "on board").
